
Antidepressant Tapering Calculator
Tapering Information
Antidepressant discontinuation syndrome is a real withdrawal reaction. A slow, monitored taper minimizes symptoms and prevents complications.
Important Safety Notes
This tool provides general information only. Always work with your healthcare provider for personalized medical advice. Never stop antidepressants abruptly.
Critical Warning: MAOIs require special caution when stopping. Abrupt discontinuation can cause severe reactions like psychosis, catatonia, or myoclonus, which require emergency care.
Never stop cold turkey: Abrupt cessation increases your risk of severe withdrawal symptoms by 3.2 times. This tool helps create a safer tapering plan.
Personalized Taper Calculator
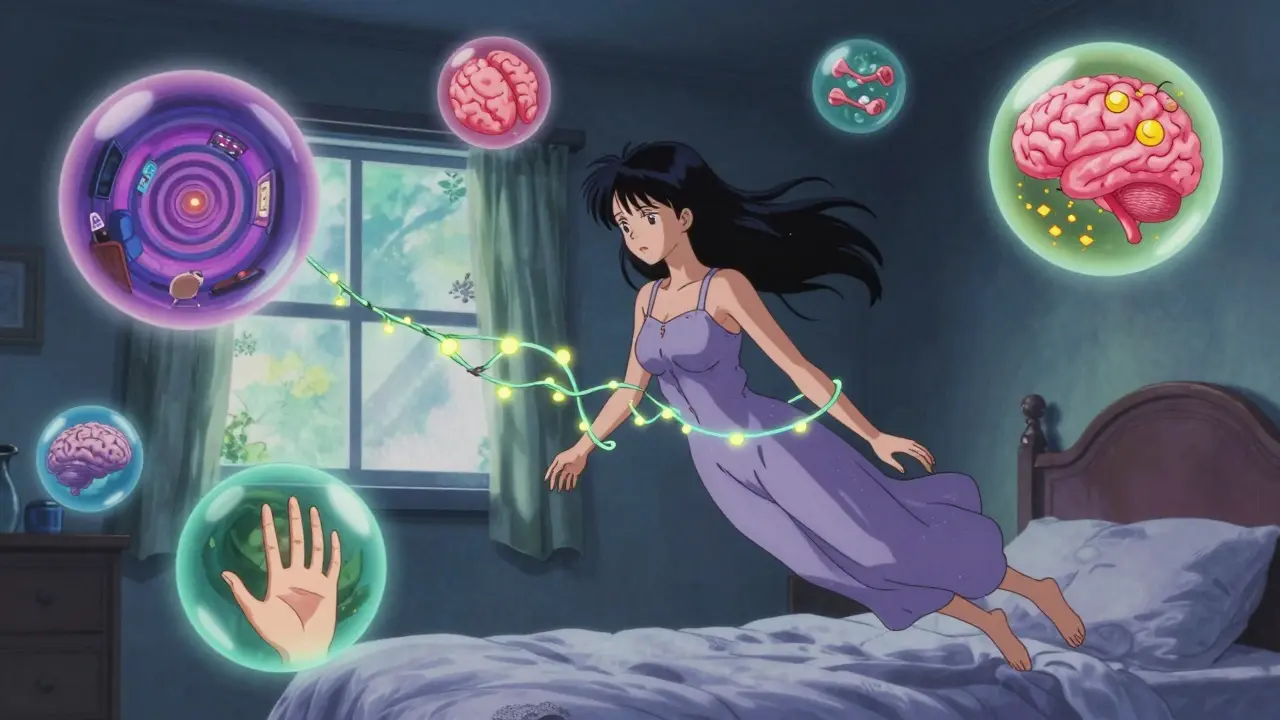
Stopping antidepressants isn’t as simple as just skipping a pill. For many people, it triggers a wave of strange, unsettling symptoms that feel like a relapse - but they’re not. This is antidepressant discontinuation syndrome, a real, physical reaction your body has to the sudden absence of a drug it’s adapted to. It’s not addiction. It’s not weakness. It’s neurobiology.
What Exactly Is Antidepressant Discontinuation Syndrome?
When you take an antidepressant - whether it’s an SSRI like sertraline or an SNRI like venlafaxine - your brain slowly adjusts. It changes how it produces, releases, and reabsorbs neurotransmitters like serotonin and norepinephrine. Over weeks or months, your nervous system gets used to the drug’s presence. When you stop suddenly, that balance collapses. Your brain hasn’t had time to readjust. The result? A withdrawal reaction. This isn’t new. The American Academy of Family Physicians recognized it back in 2006. The National Institutes of Health confirmed it in 2017. But for years, the pharmaceutical industry called it “discontinuation syndrome” to avoid the word “withdrawal,” which carries stigma. Experts like Dr. David Healy argue that’s misleading. This is a classical withdrawal syndrome - just not one tied to craving or euphoria. It’s physical dependence, plain and simple.The Symptoms: More Than Just Feeling “Off”
Symptoms usually show up within 2 to 4 days after stopping - sometimes within hours if you’re on a short-half-life drug like paroxetine or venlafaxine. They’re not subtle. Here’s what people actually report:- Flu-like feelings: Fatigue (78% of cases), muscle aches, headaches, chills, diarrhea.
- Insomnia and vivid dreams: 65% of people struggle to sleep, often with intense, disturbing dreams.
- Nausea and vomiting: 59% feel sick to their stomach - not just a little, but enough to skip meals or cancel plans.
- Dizziness and imbalance: Feeling off-balance, lightheaded, or like the room is spinning. Some describe walking like they’re drunk.
- “Brain zaps”: A sudden, electric-shock-like sensation in the head, often triggered by eye movement. Around 63% of people experience this. It’s not dangerous, but it’s terrifying the first time.
- Hyperarousal: Anxiety, agitation, irritability, panic attacks, or even anger outbursts that feel out of character.
Not All Antidepressants Are the Same
The risk and severity of withdrawal depend heavily on the drug’s half-life - how long it stays in your system.- Short half-life (high risk): Paroxetine (21 hours), venlafaxine (5-11 hours), and fluvoxamine. These cause the worst symptoms. People on venlafaxine have a 47% chance of significant withdrawal.
- Long half-life (lower risk): Fluoxetine (4-6 days). It sticks around long enough to buffer the drop, so withdrawal is often mild or absent.
It’s Not Relapse - Here’s How to Tell the Difference
This is critical. Many people - and even some doctors - mistake withdrawal for depression coming back. But here’s the key difference:- Withdrawal symptoms: Start within days of stopping. They’re physical and neurological. They get worse if you miss a dose, and they improve within 72 hours if you restart the medication.
- Relapse: Takes weeks to develop. Symptoms are emotional and psychological - low mood, hopelessness, loss of interest. Restarting the drug doesn’t fix them overnight.
How to Stop Safely: The Right Way to Taper
The only proven way to avoid or minimize withdrawal is to taper slowly. Abruptly stopping increases your risk of severe symptoms by 3.2 times.- For most SSRIs: Taper over at least 4 weeks. If you’ve been on it for over a year, go longer - 6 to 8 weeks.
- For venlafaxine or paroxetine: Use an 8-week minimum taper. Some people need 12 weeks.
- Switch to fluoxetine: If you’re on a short-half-life drug and need to stop, doctors sometimes switch you to fluoxetine first. Its long half-life makes tapering smoother.
What If Symptoms Already Started?
If you’ve already stopped and feel awful:- Don’t panic. Symptoms are temporary, even if they feel endless.
- Contact your prescriber immediately. Reintroducing the original antidepressant - even a single dose - usually clears symptoms within 72 hours.
- Don’t restart on your own. Too much can cause serotonin syndrome. Only do this under medical supervision.
Real People, Real Stories
Online communities like Surviving Antidepressants (with over 15,000 members) show a different picture than textbook descriptions. While medical literature says symptoms last 1-2 weeks, 73% of members report symptoms lasting longer than that. One person described nausea lasting three weeks after stopping sertraline. Another had brain zaps for nine months. A 2022 Reddit thread with over 1,200 comments found that 87% of people felt their symptoms were dismissed by doctors. That’s not just frustrating - it’s harmful. People end up in emergency rooms, misdiagnosed with anxiety disorders or neurological conditions, because no one connects the dots.
Special Cases: Pregnancy, Elderly, and Long-Term Use
Pregnant women often stop antidepressants without medical guidance - 41% do so on their own, according to NIH data. But abrupt cessation risks withdrawal in the mother and potential complications for the baby. Tapering under a specialist’s care is safer. For older adults, withdrawal can mimic dementia or stroke - dizziness, confusion, balance issues. Doctors may misattribute these to aging. Always mention your medication history. If you’ve been on antidepressants for years, your brain has adapted deeply. A slow taper isn’t optional - it’s essential. Rushing this can lead to protracted withdrawal, where symptoms linger for months or even over a year. Recent studies show 18.7% of people discontinuing SSRIs have symptoms beyond three months.What’s Next? Research and Hope
Scientists are now studying biomarkers to predict who’s at risk. Clinical trials (NCT04567890, NCT04812345) are testing personalized tapering protocols. The Royal College of Psychiatrists updated its guidelines in 2022 to acknowledge protracted withdrawal as a real clinical phenomenon. The message is clear: antidepressants aren’t harmless. Stopping them requires the same care as stopping benzodiazepines or alcohol. You wouldn’t quit those cold turkey. Don’t do it with antidepressants either.What to Do If You’re Thinking About Stopping
1. Don’t decide alone. Talk to your doctor - not just your pharmacist or a quick online consultation. 2. Ask about your drug’s half-life. Is it short or long? That determines your taper speed. 3. Plan the taper. Don’t wing it. Write down your schedule: “Reduce by 10% every 10 days.” 4. Track your symptoms. Use a simple journal: date, dose, symptoms, mood. This helps your doctor spot patterns. 5. Have a backup plan. If symptoms hit hard, know how to reach your prescriber fast. You’re not broken. You’re not weak. You’re just human - and your nervous system is trying to heal. Give it the time it needs.Can antidepressant withdrawal be dangerous?
Yes, in rare cases. While most symptoms are uncomfortable but not life-threatening, stopping MAOIs abruptly can trigger severe reactions like psychosis, catatonia, or myoclonus. These require emergency care. Even with SSRIs or SNRIs, sudden withdrawal can cause intense anxiety, suicidal thoughts, or severe imbalance that increases fall risk. Always taper under medical supervision.
How long do antidepressant withdrawal symptoms last?
For most people, symptoms last 1-2 weeks and resolve on their own. But research and patient reports show that 18-28% experience symptoms lasting longer - sometimes months or over a year. This is called protracted withdrawal. It’s less common, but it’s real. The longer you’ve been on the medication and the faster you stopped, the higher the risk.
Why do I get brain zaps when I move my eyes?
Brain zaps are believed to be caused by sudden changes in serotonin signaling in the brainstem and sensory pathways. Eye movements trigger neural activity that, in a destabilized system, creates brief electrical misfires. They’re not seizures or neurological damage - just a sign your brain is rewiring. They usually fade as your nervous system stabilizes.
Can I switch to a different antidepressant to avoid withdrawal?
Sometimes, yes. Switching from a short-half-life drug like paroxetine to fluoxetine (which has a long half-life) can make tapering smoother. This is called a “cross-taper.” But it’s not risk-free - mixing antidepressants can cause serotonin syndrome. Only do this under strict medical supervision with careful dosing.
Is it safe to stop antidepressants during pregnancy?
It’s possible, but not without planning. About 41% of pregnant women stop antidepressants on their own, often out of fear. But abrupt cessation can trigger withdrawal symptoms that affect both mother and baby. A slow, monitored taper - or switching to a safer medication like sertraline - is usually preferred over sudden stopping. Always work with a perinatal psychiatrist.
Will I ever feel normal again after stopping?
Yes - for the vast majority, symptoms fade completely. Even people with protracted withdrawal report gradual improvement over months. Your brain is resilient. It rewires itself. But recovery takes time. Focus on sleep, nutrition, gentle movement, and stress reduction. Avoid alcohol and caffeine. Most people return to baseline within 6-12 months, even after long-term use.




Gabrielle Panchev
January 5, 2026 AT 12:44Saylor Frye
January 7, 2026 AT 00:29Beth Templeton
January 8, 2026 AT 18:48Dana Termini
January 10, 2026 AT 13:31Wesley Pereira
January 11, 2026 AT 06:30Isaac Jules
January 12, 2026 AT 01:22Amy Le
January 13, 2026 AT 06:44Pavan Vora
January 14, 2026 AT 18:45Indra Triawan
January 16, 2026 AT 01:20Lily Lilyy
January 16, 2026 AT 06:16Susan Arlene
January 17, 2026 AT 22:13Joann Absi
January 18, 2026 AT 10:01Mukesh Pareek
January 18, 2026 AT 19:45Molly McLane
January 20, 2026 AT 05:10