
Trying for a baby and hitting a dead end can feel like running a marathon and tripping right before the finish line. The moment doctors mention 'infertility', your world flips. Suddenly, every bit of hope is precious. That’s why so many couples end up talking about Clomid, a medication that’s buzzed about for helping with fertility roadblocks. But what really makes Clomid tick—and does it deserve all the hype? The stories and data might surprise you.
The Science Behind Clomid: What It Does and How It Works
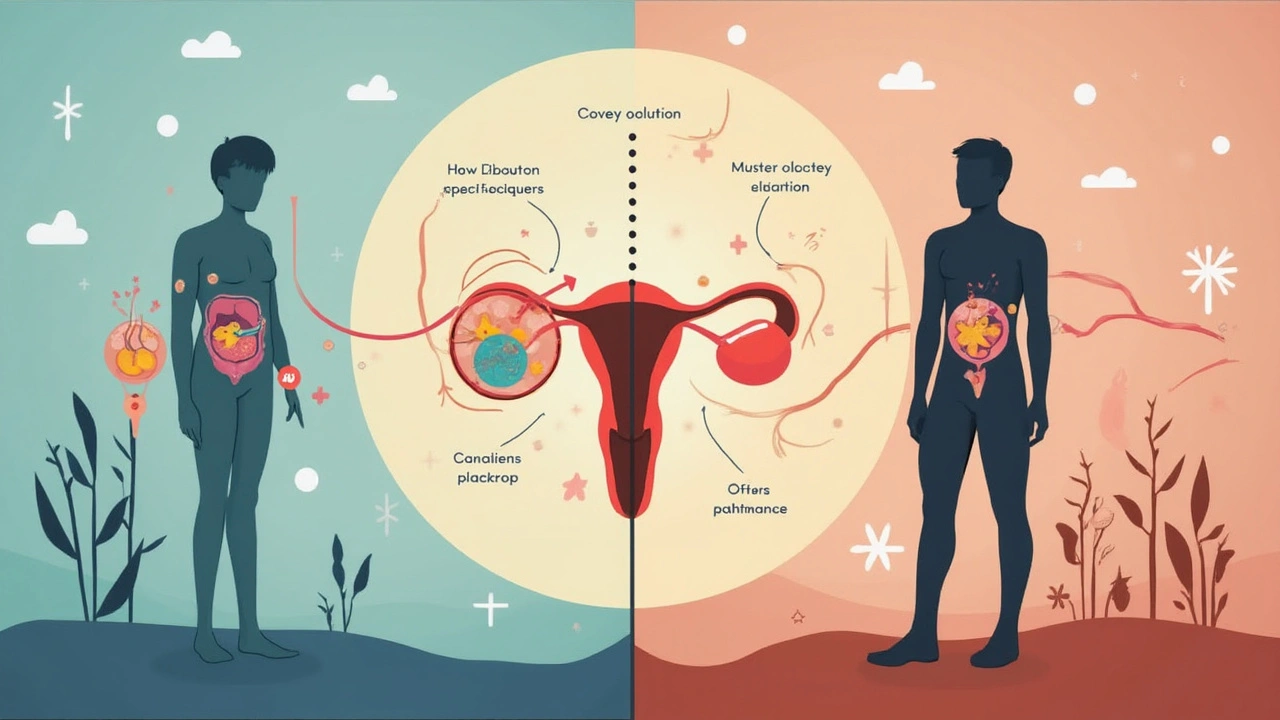
Clomid, or clomiphene citrate, isn’t just another prescription lining the pharmacy shelves. Its magic lies in its ability to boost natural hormones that are essential for fertility. It was first approved by the FDA back in 1967, but the basic idea hasn’t changed much: Clomid makes your body release more eggs than usual. For women struggling with ovulation, this is a real game-changer. The drug acts by blocking estrogen receptors in the brain, essentially tricking the brain into thinking there’s less estrogen than there truly is. What happens next? The pituitary gland releases more gonadotropins, especially follicle-stimulating hormone (FSH) and luteinizing hormone (LH). These are the hormones that fire up the ovaries, leading to the release of eggs (ovulation).
But here’s where it gets even more interesting: doctors sometimes use Clomid for male infertility too. Sounds odd, right? For men, the same trick—blocking estrogen—nudges the testes to ramp up testosterone production and crank out more sperm. It’s a smart workaround, especially for men with borderline or unexplained low sperm counts. According to a 2021 study in "Human Reproduction Update," Clomid increased sperm concentration in men by about 50% on average after three months of daily use. That’s a stat worth paying attention to if you’ve been told male fertility is at fault.
While the usual Clomid prescription for women is 50mg daily for five days early in the menstrual cycle, men often get lower, steady doses over a few months. There’s a catch, though: Clomid isn’t a miracle cure for everyone. About 70-80% of women who take it start ovulating, but only about 40% will become pregnant in the first six months. That means patience is part of the journey.
Why and When Doctors Prescribe Clomid
Clomid is the frontline pick for women who don’t ovulate regularly, often because of conditions like polycystic ovary syndrome (PCOS). But doctors also turn to it for women with irregular periods or unexplained infertility. Before even talking about Clomid, though, they’ll run some basic tests: hormone levels, ultrasounds of the ovaries, and, less often, check the male partner’s sperm count.
If you’re a woman under 35 who’s been trying for a year, or over 35 and trying for six months, doctors may start the Clomid conversation. They’ll usually run through a routine like this:
- Start Clomid on day 3, 4, or 5 of your menstrual cycle
- Take one pill (usually 50mg) daily for five days
- Watch for ovulation between days 10 and 17 using ovulation predictor kits or ultrasounds
- Track side effects and hormone levels with blood tests
If you ovulate but still don’t get pregnant after several months, doctors may up the dose, add another medication (like metformin if you have PCOS), or refer you to more advanced fertility treatments. For men, the process is slower but pretty straightforward—usually 25-50mg every other day, with semen analysis checks every few months.
Some doctors still hold off on Clomid if there are bigger hurdles, like blocked fallopian tubes, severe endometriosis, or if male sperm counts are basically zero. It’s not going to fix mechanical problems or chromosomal issues.
Clomid Side Effects, Risks, and What To Expect
Most people think fertility drugs are all unicorns and rainbows until they start taking them, then reality hits. Clomid can trigger a handful of annoying, sometimes intense, side effects:
- Hot flashes (like your own personal sauna—about 1 in 10 women will get them)
- Headaches and mood swings (ranging from feeling extra weepy to random anger)
- Breast tenderness and bloating
- Visual disturbances (though rare, some people see flashing lights or spots)
About 5-10% of women end up with twins after taking Clomid—compare that to a 1% chance of twins with natural conception. Triplets or more are rare, but still a small risk, so you can’t rule it out. Ovarian hyperstimulation syndrome (OHSS) is another possible risk, but it’s less common with Clomid than with stronger injectable hormones.
For men, side effects tend to be milder—headaches, occasional moodiness, and sometimes a dip in libido. Most studies say Clomid’s risk profile is pretty gentle compared to other infertility treatments, with the biggest concern being that not everyone responds as hoped. After about six months to a year, if there’s no good news, doctors recommend switching gears.
| Clomid Side Effect | Estimated Likelihood |
|---|---|
| Hot Flashes | 10-20% |
| Mood swings | Up to 50% |
| Headache | 2-7% |
| Twins or multiples | 5-12% |
| Vision changes | 1-2% |
Doctors always warn patients not to stay on Clomid forever. Long-term use doesn’t make the drug any more effective and could actually cause problems with thin uterine lining or hostile cervical mucus, making it harder—not easier—to get pregnant. Most clinics stop after about six cycles.
Clearing Up Myths and Misconceptions Around Clomid
There’s so much chatter about Clomid online—some right, some way off base. First, Clomid won’t 'guarantee' a pregnancy. You still need eggs, sperm, and open fallopian tubes for anything to happen. It doesn’t fix broken tubes or severe sperm problems—think of it more as a gentle accelerator, not the whole car.
Another rumor is that Clomid always causes twins or triplets. The truth? Twins are more likely, but most pregnancies after Clomid are singletons. The 'triplet or more' scenario is only about 1 in 500. Also, men sometimes worry that Clomid will make them less masculine because it blocks estrogen. That’s not how it works—in fact, low-dose Clomid actually raises testosterone in men with certain types of infertility, which can even make them feel better in other ways.
And what about mood swings? Yes, some folks get emotional, but others barely notice. If you’re prone to anxiety or depression, tell your doctor—don’t suffer in silence. Sometimes just knowing what’s ahead makes it less scary.
People also swap stories about Clomid 'thinning the uterine lining.' Studies do show that a small group of women may notice this after several cycles, but most don’t have issues unless Clomid is used for too long. If it pops up, doctors can switch meds or use estrogen supplements. It’s not game over.

Tips and Real-World Advice for Clomid Users
If you’re about to take Clomid—or your partner is—here’s what nobody tells you in the pharmacy line. First, get your timing right. Ovulation usually happens about 7-10 days after the last pill, so daily ovulation predictor tests are useful. Mark your calendar and watch for those positive results, especially if you want to catch your most fertile days.
Track side effects in a journal or with an app. If you start feeling off, jot it down. Patterns matter, and your doctor will want those details if things get weird. Stay hydrated, especially if you notice headaches or bloating—water helps more than you’d think.
Sex can feel like a chore when you’re 'scheduled' around ovulation. Try to keep things fun, even silly, if possible. A recent survey from the American Society for Reproductive Medicine found that stress can drop the odds of conception—so anything that lightens the mood helps more than any pill.
If you don’t get pregnant after 4-6 cycles, don’t panic. Some couples just need more time or a different approach. Ask your doctor about next steps: sometimes it means trying intrauterine insemination (IUI) or in vitro fertilization (IVF). And if you’re a guy on Clomid, keep an eye on your sperm counts—if they aren’t budging, your doctor may tweak the dose or check for other issues like varicoceles or hormone problems.
- Avoid over-the-counter supplements that claim to 'boost fertility' unless your doctor approves. Some actually mess with hormone levels and hurt your chances instead of helping.
- Stay active. Gentle exercise helps hormone regulation, boosts mood, and keeps you grounded during the wild ride of trying to conceive.
- Talk openly with your partner. The emotional load can get heavy quickly, and having a solid support system is key.
Remember, every fertility story is different. Some couples succeed on the first round, others after months or more. Clomid opens the door, but sometimes you need patience—plus a dash of flexibility—to walk through it. Keep asking questions and trust your gut along the way.



Philip Crider
May 31, 2025 AT 08:49Jackie Burton
May 31, 2025 AT 19:44Diana Sabillon
June 2, 2025 AT 07:28neville grimshaw
June 2, 2025 AT 23:57Carl Gallagher
June 4, 2025 AT 05:58bert wallace
June 4, 2025 AT 17:37Neal Shaw
June 5, 2025 AT 09:06Hamza Asghar
June 5, 2025 AT 15:43Karla Luis
June 7, 2025 AT 01:39jon sanctus
June 9, 2025 AT 00:03Kenneth Narvaez
June 9, 2025 AT 21:02Christian Mutti
June 10, 2025 AT 22:55