Why Reducing Medications Isn’t Just Stopping Pills
Most people assume that taking more medications means better health. But for older adults juggling five, ten, or even more prescriptions, that’s often not true. In fact, too many drugs can be dangerous. Deprescribing isn’t about cutting corners-it’s about removing what no longer helps and might be hurting. This isn’t a new idea, but recent research is finally showing what happens when doctors and patients work together to safely reduce unnecessary meds.
The Real Problem: Too Many Pills, Too Little Benefit
In the U.S., 40% of adults over 65 take five or more medications daily. One in five take ten or more. Many of these drugs were prescribed years ago-for high blood pressure, cholesterol, or acid reflux-when the patient was healthier. Now, their body has changed. Their kidneys don’t filter as well. Their liver slows down. Their goals have shifted from living longer to living better. But the pills keep coming.
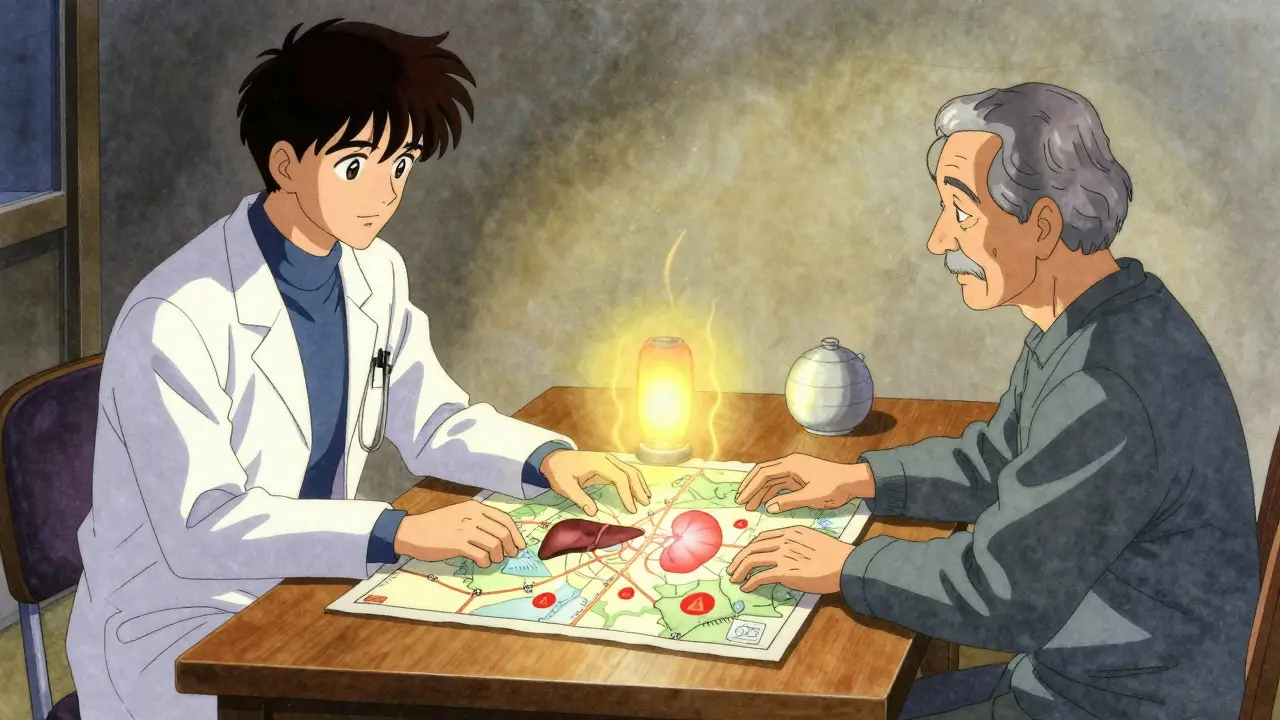
That’s where deprescribing steps in. It’s not about stopping all meds. It’s about asking: Is this still helping? The American Geriatrics Society defines it as the planned, supervised process of reducing or stopping drugs that may cause more harm than good. This isn’t guesswork. It’s a clinical process with five clear steps: identify risky meds, decide if they can be cut, plan a taper, watch for withdrawal or return of symptoms, and document everything.
What Happens When You Actually Reduce Medications?
Research from JAMA Network Open in 2023 looked at over 50 studies involving older adults with polypharmacy. The results? On average, deprescribing cut the number of medications per person by about one. Sounds small? It’s not. For a doctor with 2,000 patients, that’s 140 fewer pills being taken every day. That’s 140 fewer chances for falls, confusion, stomach bleeding, or kidney damage.
But the real win isn’t just fewer pills-it’s fewer hospital visits. Studies show deprescribing reduces falls by up to 25% in frail older adults, especially when stopping sedatives, antipsychotics, or blood pressure drugs that cause dizziness. Mental clarity improves when benzodiazepines or sleep aids are slowly removed. One trial found patients reported better sleep, less grogginess, and more energy after stopping long-term proton pump inhibitors (PPIs) they didn’t need anymore.
And yes-some people worry about symptoms coming back. That’s why tapering matters. Stopping a blood pressure pill cold turkey can be dangerous. But slowly lowering the dose over weeks, while monitoring blood pressure at home, often shows the body adjusts fine. In fact, many patients find their symptoms don’t return at all.
Why Don’t More Doctors Do This?
Here’s the uncomfortable truth: doctors rarely bring it up. Patients don’t ask. Why? Because we’ve been trained to think more drugs = better care. And patients often feel guilty if they question their prescriptions. One study found that 80% of older adults would be open to reducing meds-if their doctor started the conversation.
But most doctors don’t know how. They’re pressed for time. They’re worried about liability. They’re not sure what to cut. That’s changing. The American Academy of Family Physicians is now building tools that plug into electronic health records to flag high-risk meds automatically. In pilot clinics, this led to a 15% drop in inappropriate prescriptions within six months.
Another barrier? Hospital stays are too short. A patient might get 10 new meds while hospitalized for pneumonia. When they’re discharged, no one checks if those meds are still needed. That’s why collaboration between hospitals and primary care is critical. The best outcomes happen when the family doctor reviews the full list after discharge.
Who Benefits Most From Deprescribing?
Not everyone needs it. But certain groups see the biggest gains:
- Older adults with frailty or dementia
- Those with advanced illness or limited life expectancy
- People taking multiple drugs that affect the brain-like sleeping pills, anti-anxiety meds, or antipsychotics
- Patients on preventive drugs (like statins or aspirin) with no clear short-term benefit
- Anyone who’s had a fall, confusion, or unexplained fatigue recently
For example, a 78-year-old woman with mild dementia and high blood pressure was on eight medications. She was falling weekly. Her doctor removed a sleep aid, a mild antidepressant, and a daily aspirin she’d been taking for 15 years. Within three months, her falls stopped. Her memory didn’t get worse. She felt more alert. She was on five meds. That’s not losing care-it’s gaining quality.

What the Research Still Doesn’t Tell Us
There’s a gap. Most deprescribing studies last only 6 to 12 months. We don’t know what happens after five years. Do people stay off those meds? Do they live longer? Do they have fewer heart attacks or strokes? We need longer studies with real outcomes-not just pill counts.
Also, we don’t have good tools to predict who will do well. Some people can stop a blood thinner safely. Others can’t. Genetics might play a role. Early research is looking at how people metabolize drugs like benzodiazepines or PPIs based on their DNA. That could one day help personalize deprescribing-making it safer and more precise.
How Patients Can Start the Conversation
You don’t need to wait for your doctor to bring it up. If you’re taking five or more meds and feel tired, confused, or unsteady, ask:
- “Is this medicine still helping me?”
- “What happens if I stop taking it?”
- “Are there any side effects I might not notice?”
- “Can we try cutting one at a time?”
Use resources like deprescribing.org. They offer printable checklists and questions to bring to appointments. One patient in New Zealand brought a list of her 12 meds to her GP. Together, they removed four-no side effects, better sleep, less bloating. She didn’t lose care. She got back control.
It’s Not About Cutting Costs-It’s About Cutting Risk
Yes, deprescribing saves money. A single pill cut from a long-term regimen can save hundreds a year. But that’s not the point. The point is safety. The point is dignity. The point is helping people live without being weighed down by pills they don’t need.
Deprescribing isn’t the opposite of prescribing. It’s its mirror image. Just as we carefully choose when to start a drug, we must be just as careful when to stop. And now, with better guidelines, better tools, and growing evidence, it’s not just possible-it’s responsible care.




Gaurav Meena
January 31, 2026 AT 04:23Beth Beltway
January 31, 2026 AT 19:33Natasha Plebani
February 2, 2026 AT 16:06Rob Webber
February 2, 2026 AT 21:32Yanaton Whittaker
February 4, 2026 AT 11:15Kathleen Riley
February 6, 2026 AT 00:52Beth Cooper
February 6, 2026 AT 08:10Lily Steele
February 7, 2026 AT 16:12Bobbi Van Riet
February 7, 2026 AT 22:07Sazzy De
February 7, 2026 AT 23:50Blair Kelly
February 9, 2026 AT 16:19Rohit Kumar
February 10, 2026 AT 08:28Katie and Nathan Milburn
February 12, 2026 AT 02:47