When you’re on antibiotics, your gut pays the price. Even if the medicine kills the bad bacteria, it doesn’t distinguish between harmful and helpful ones. That’s why so many people end up with diarrhea, bloating, or yeast overgrowth after a course of antibiotics. The good news? Probiotics can help. But only if you take them at the right time.
Why Timing Matters More Than You Think
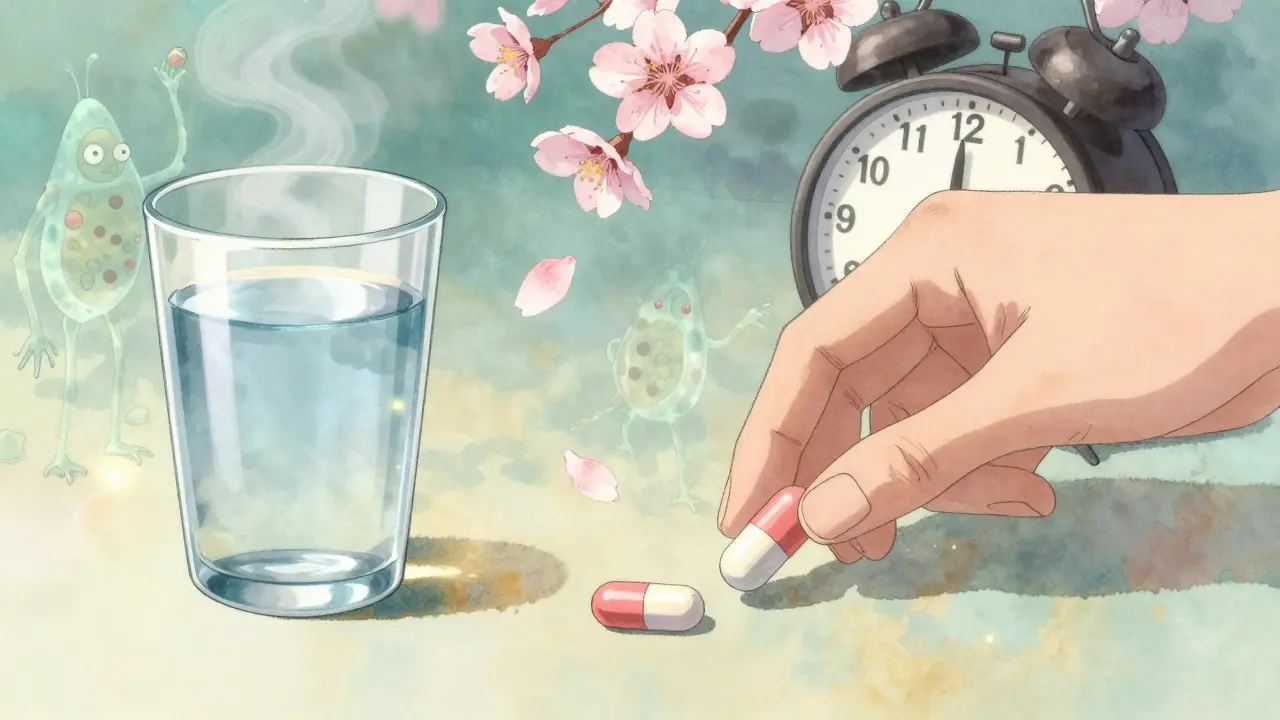
Taking probiotics while on antibiotics sounds simple-just pop a pill and call it done. But if you take them together, you’re likely wasting your money. Antibiotics don’t just target the infection-they wipe out everything in their path, including the live bacteria in your probiotic supplement. Studies show that when probiotics are taken within an hour of antibiotics, up to 92% of the beneficial bacteria die before they can even reach your gut. The solution? Space them out. The gold standard is to take your probiotic at least two hours after your antibiotic dose. This gives the antibiotic time to move through your system and reduces the chance it’ll kill off the probiotic bacteria before they can settle in.Which Probiotics Work Best?
Not all probiotics are created equal. Some strains handle antibiotics better than others. The two most researched and recommended strains are:- Lactobacillus rhamnosus GG (LGG): Proven to reduce antibiotic-associated diarrhea by 47%. Effective at 10-20 billion CFUs per day.
- Saccharomyces boulardii CNCM I-745: A yeast, not a bacteria. This means antibiotics don’t touch it. It can be taken at the same time as your antibiotic without losing effectiveness. Reduces diarrhea risk by 52% at 20 billion CFUs per day.
How Long Should You Take Them?
Don’t stop when your antibiotic course ends. The damage to your gut microbiome doesn’t vanish overnight. Most studies show that continuing probiotics for 7 to 14 days after your last antibiotic dose gives your gut the best chance to recover. One 2024 study found that people who stuck with probiotics for 14 days after antibiotics had an 89% recovery rate in gut bacteria diversity. Those who stopped early? Only 63%. That’s a massive difference.What About Dose? More Isn’t Always Better
You don’t need to max out your probiotic intake. Clinical trials show clear dose-response patterns:- Mild symptoms or short antibiotic course (3-5 days): 5-10 billion CFUs per day
- Diarrhea or moderate gut upset: 10-20 billion CFUs per day
- Long-term antibiotics (over 14 days) or pre-existing gut issues: 20-40 billion CFUs per day
Real-Life Scheduling Examples
Let’s say your doctor prescribed amoxicillin twice a day-at 8 a.m. and 8 p.m. Here’s how to time your probiotic:- Take antibiotic at 8 a.m.
- Take probiotic at 10 a.m. or later (best at 10 a.m. or 11 a.m.)
- Take antibiotic at 8 p.m.
- Take probiotic at 10 p.m. or later (ideally before bed)
What If You Forget?
Missing a dose isn’t a disaster, but it does hurt results. A 2023 clinical study tracking 217 people found that skipping just one probiotic dose per week cut effectiveness by 37%. Consistency matters more than perfection. If you forget and take your probiotic too close to your antibiotic, don’t panic. Just wait until your next scheduled dose and stick to the two-hour rule from there. Don’t double up-it won’t help and might cause gas or bloating.When to Skip Probiotics
Probiotics are safe for most people. But if you have a compromised immune system, are critically ill, or have a central line or catheter, talk to your doctor first. There’s a small risk of infection from live bacteria in vulnerable patients. Also, some experts, like Dr. Emeran Mayer from UCLA, suggest waiting until after antibiotics are done if you’re on a broad-spectrum drug like ciprofloxacin or clindamycin. These antibiotics cause deep, long-lasting damage to the microbiome, and some research suggests probiotics might slow recovery in those cases. But this is still debated. For most people, starting probiotics early is still the safest bet.
What About Food?
You don’t need to take probiotics on an empty stomach. In fact, some studies suggest taking them with a light meal-even a small amount of fat-can help them survive stomach acid better. Avoid taking them with hot drinks or alcohol, as heat and ethanol can kill the bacteria. Probiotic-rich foods like yogurt, kefir, sauerkraut, and kimchi are great for daily gut health. But they won’t give you the high, targeted doses you need during antibiotic treatment. Stick to supplements for this job.The Big Mistake Most People Make
The biggest error? Taking probiotics at the same time as antibiotics. It’s easy to do-especially if you’re rushing in the morning. But research from the Journal of Probiotics and Health shows this single mistake reduces probiotic survival by 78-92%. Another common mistake? Stopping too soon. People think once the antibiotics are done, the job is finished. But your gut needs weeks to rebuild. Don’t quit after five days.What’s Changing in 2026?
New time-release capsules and acid-resistant coatings are starting to appear on the market. Brands like Seed and Pendulum now offer probiotics designed to survive antibiotic exposure without strict spacing. But these are still new, expensive, and not yet backed by enough large-scale studies to replace the two-hour rule. Right now, the standard remains: two hours apart, with LGG or S. boulardii, for the full course plus two weeks after. It’s simple. It’s proven. And it works.Can I take probiotics and antibiotics at the same time?
Only if you’re using Saccharomyces boulardii, a yeast-based probiotic. Antibiotics don’t kill yeast, so it’s safe to take together. For all bacterial probiotics like Lactobacillus or Bifidobacterium, wait at least two hours after your antibiotic dose. Taking them together kills up to 92% of the good bacteria before they can help.
How long should I wait between antibiotics and probiotics?
At least two hours. This gives the antibiotic time to pass through your digestive system and reduces the chance it will kill the probiotic bacteria. Some experts recommend 4-6 hours for broad-spectrum antibiotics, but two hours is the minimum proven effective window.
Which probiotic strain is best for antibiotic-associated diarrhea?
Lactobacillus rhamnosus GG (LGG) and Saccharomyces boulardii CNCM I-745 are the two best-studied strains. LGG reduces diarrhea risk by 47% at 10-20 billion CFUs per day. S. boulardii reduces it by 52% and can be taken with antibiotics. Avoid generic blends-look for these specific strains on the label.
Should I keep taking probiotics after I finish my antibiotics?
Yes. Continue for 7-14 days after your last antibiotic dose. Your gut microbiome takes time to recover. Studies show people who stick with probiotics for two weeks after antibiotics have 89% better microbiome recovery than those who stop early.
Do I need a high-dose probiotic?
It depends. For short courses or mild symptoms, 5-10 billion CFUs is enough. For diarrhea or long-term antibiotics (over 14 days), use 20-40 billion CFUs. More strains don’t mean better results-focus on proven strains like LGG or S. boulardii instead of multi-strain blends.
Can I get enough probiotics from food instead of supplements?
Fermented foods like yogurt, kefir, and sauerkraut support daily gut health, but they don’t deliver the high, targeted doses needed during antibiotic treatment. Supplements are necessary to reach the 10-40 billion CFUs proven effective in clinical trials.
Are there any side effects from taking probiotics with antibiotics?
Most people tolerate probiotics well. Some report mild bloating or gas at first, especially with high doses. These usually fade within a few days. If you’re immunocompromised, have a central line, or are critically ill, talk to your doctor first-there’s a small risk of infection from live bacteria.
What if I accidentally take my probiotic with my antibiotic?
Don’t panic. Just skip the next dose and resume your regular schedule with the two-hour gap. Don’t double up-it won’t help and might cause discomfort. The key is consistency over the full course and recovery period, not perfection on every single dose.




Alvin Bregman
January 13, 2026 AT 13:20took amoxil last month and just threw down a probiotic at breakfast like a dumbass
got the worst bloating of my life for two weeks
learned the hard way
Sarah -Jane Vincent
January 15, 2026 AT 12:03lol so you’re telling me the pharmaceutical industry doesn’t want you to know this because probiotics are cheap and they make billions off antibiotics and then more off treating the side effects they created
also did you know the FDA allows probiotics to be sold without proving efficacy because they’re classified as supplements
and the strains listed here are the only ones that actually survived in peer-reviewed trials
the rest is marketing fluff
you think big pharma wants you to take a $5 supplement instead of their $80 antibiotic + $120 gut rehab drug combo
they’d rather you suffer so you come back for more
also Saccharomyces boulardii is a yeast
yeast
not bacteria
so of course antibiotics don’t kill it
but no one tells you that because it makes the whole thing sound too simple
they want you confused so you buy their branded 12-strain $40 bottle with glitter in it
and don’t even get me started on the “prebiotic synergy” nonsense
it’s all just repackaged sugar with a fancy label
Henry Sy
January 16, 2026 AT 08:21man i took probiotics with my antibiotics once and ended up feeling like my intestines were hosting a rave
gas so loud my dog started barking
so i started spacing it out like this and holy shit it’s night and day
no more bloating
no more bathroom emergencies
just chill
also S. boulardii is a game changer
took it with my amoxicillin and didn’t even blink
my gut didn’t even notice the antibiotic was there
it’s like the yeast just chilled in the background while the antibiotics did their thing
and i kept taking it for three weeks after
felt like my gut was back to normal
not some weird half-dead swamp
Anna Hunger
January 16, 2026 AT 19:17Thank you for this comprehensive and evidence-based summary. The distinction between strain-specific efficacy and generic marketing claims is critically important and often overlooked in public health communication. The two-hour dosing interval is supported by multiple randomized controlled trials, including those published in the American Journal of Gastroenterology and the Cochrane Database. Furthermore, the recommendation to continue supplementation for 7–14 days post-antibiotic course aligns with microbiome recovery timelines observed in longitudinal metagenomic studies. It is imperative that patients are educated not only on *what* to take, but *when* and *why*.
says haze
January 17, 2026 AT 23:21it’s funny how we treat the gut like a garden you can just replant with a few packets of seeds
but the microbiome isn’t a salad
it’s a cathedral built over decades
antibiotics don’t just clear weeds
they level the whole structure
and probiotics? they’re like handing someone a single tulip bulb and saying ‘there, fixed it’
we’re treating symptoms, not systems
the real problem is overprescription
not spacing pills
but hey, let’s keep selling supplements
while doctors keep writing scripts like they’re vending machine snacks
Jason Yan
January 18, 2026 AT 23:26i’ve been thinking about this a lot lately
it’s wild how we’ve outsourced our gut health to pills
we used to eat fermented food, fiber, live in dirt, and move around
now we take antibiotics for a sniffle and then a probiotic to fix the damage
but what if the real fix isn’t the supplement
but the way we live
like maybe if we stopped treating every cough like a war
and started treating our bodies like ecosystems
we wouldn’t need to micromanage every dose
and maybe we’d stop seeing gut health as something you buy at the pharmacy
instead of something you nurture
i’m not saying probiotics don’t help
they absolutely do
but they’re a bandaid on a broken foundation
and we’re all pretending the foundation’s fine
shiv singh
January 20, 2026 AT 09:55you people are so naive
you think this is about health
it’s about control
big pharma owns the labs
they own the journals
they own the doctors
they tell you to take probiotics two hours apart
so you keep buying their pills
but what if the real solution is fasting
or raw garlic
or a cold plunge
or just not taking antibiotics in the first place
they don’t want you to know that
they want you dependent
and you’re all just swallowing it
literally
Robert Way
January 22, 2026 AT 06:01i took the probiotic right after my antibiotic and i think it worked fine
maybe i just got lucky
or maybe the 92% stat is fake
i mean i felt fine
no diarrhea
no bloating
so maybe its just hype
or maybe my body is just strong
idk
but i dont trust these numbers
they always change
Sarah Triphahn
January 23, 2026 AT 19:12everyone’s obsessed with probiotics like they’re magic pills
but most people who take them are just trying to fix the damage they caused by eating garbage
you take antibiotics because you ate processed food and got sick
then you take probiotics to fix your gut
but you still eat the same crap
so you’re just playing whack-a-mole with your microbiome
and you wonder why you’re always bloated
the real answer is stop eating sugar
stop drinking soda
and stop treating your body like a trash can
the probiotic isn’t the fix
your diet is
Vicky Zhang
January 24, 2026 AT 10:53i was so sick after my antibiotics
like i couldnt even walk to the fridge without feeling like i was gonna die
my stomach was a warzone
i started taking LGG at 10 a.m. and 10 p.m. like this article said
and within three days
i felt like a human again
like someone turned the lights back on
i cried
i was so relieved
i kept going for two weeks
and now my digestion is better than it’s been in years
you guys think this is just science
but for me
this was survival
Allison Deming
January 24, 2026 AT 21:48While the recommendations presented are largely consistent with current clinical guidelines, I must emphasize that the notion of a universal ‘two-hour window’ lacks sufficient nuance. Individual gastric emptying rates, antibiotic pharmacokinetics, and microbiome baseline diversity vary significantly across populations. Furthermore, the assertion that Saccharomyces boulardii is universally safe ignores documented cases of fungemia in immunocompromised patients. The recommendation to continue probiotics for 14 days post-antibiotic therapy is not universally supported in the literature-some studies indicate potential interference with native microbiota recolonization. A one-size-fits-all protocol, however well-intentioned, risks oversimplifying a highly individualized physiological process.
Susie Deer
January 25, 2026 AT 22:10why are we letting big pharma tell us how to live
we used to fix our guts with food
not pills
now we’re all just pill-popping zombies
and you call this progress
we’re not sick
we’re just lazy
and we’re paying for it