
When you first hear the name Effexor, maybe it sounds almost sci-fi, but the reality is much more down-to-earth. Effexor is everywhere. GPs mention it, psychiatrists recommend it, and you might even know someone quietly taking it. But what’s surprising is how few people understand what Effexor actually does or why it’s become such a go-to for dealing with anxiety and depression. Grab a cup of coffee or whatever helps, because what’s underneath that bright orange bottle is a story about the way we treat mental health in 2025—a mix of hope, hard science, and a decent amount of confusion.
What Exactly Is Effexor and How Does It Work?
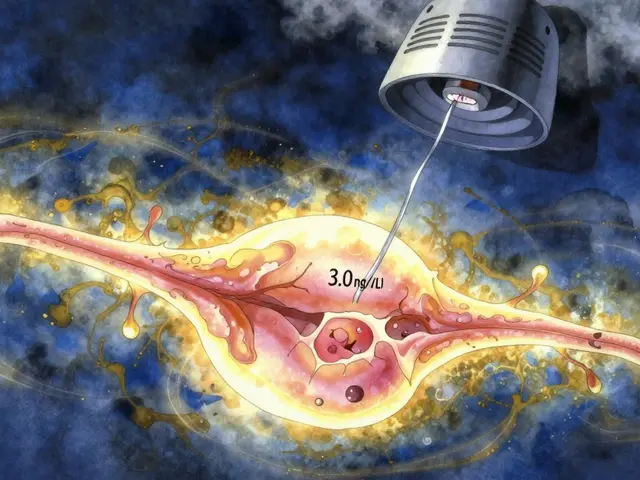
Effexor is the brand name for venlafaxine, a medication doctors reach for when someone’s struggling with depression, anxiety, panic, or even ongoing nerve pain. It’s a member of the “SNRI” family. That stands for serotonin and norepinephrine reuptake inhibitor. Sounds intimidating, but here’s what’s actually happening: inside your brain, nerves send signals using chemical messengers called neurotransmitters. Serotonin and norepinephrine are two big ones. Picture a bunch of tiny boats (neurotransmitters) floating across a river (your brain’s synapses), carrying good vibes between islands. When things aren’t quite right, these chemical boats don’t make enough trips—or get sucked back before doing their job. Effexor helps keep those boats on course, letting more of those mood-boosting messengers stick around.
Here in New Zealand, pharmacies fill thousands of Effexor scripts each week. The (very recent) 2023 New Zealand General Practice Study found about 4.8% of the adult population had tried an SNRI, most of them Effexor. The main reason? It often works when classic SSRIs like fluoxetine or sertraline don’t do enough. The dual approach—tackling both serotonin and norepinephrine—can mean a stronger or steadier lift out of mood slumps or overwhelming anxiety. Australians and Canadians also use plenty of it. Across different age groups, it’s quietly quarterbacking many recovery stories, especially for folks whose brains just don’t respond to milder meds.
But it’s not magic. Effexor needs around 2–6 weeks (sometimes even longer) to kick in. That’s one of its biggest frustrations—waiting for signs that it’s actually doing the heavy lifting. During this waiting game, symptoms might feel the same or, for some, briefly worsen before getting better. Some people feel a sudden improvement, like a wall finally coming down. Others notice subtle, gradual shifts—a little more energy, a bit of that constant worry starting to ease, or maybe just the ability to get out of bed without a fight. It’s all deeply personal, which itself can be endlessly confusing.
Dosing is another puzzle. Effexor XR (the extended-release version) is the most popular in 2025, because it smooths out the delivery and lowers the risk of sharp peaks or valleys in your mood. The range is usually between 75 and 225mg per day for depression, and sometimes up to 375mg for more stubborn cases. Some people find relief with half that. The right dose isn’t one-size-fits-all; it’s about balancing symptom relief with the least side effects. You might hear people comparing notes, talking about how "150mg was my sweet spot," while another says, "Couldn’t handle more than 112.5mg." Everyone’s brain is a unique beast.
If you’re wondering whether it’s safe to drink a glass of wine with Effexor, doctors usually say to keep it very minimal. Alcohol can ramp up side effects, particularly drowsiness and poor coordination. One Auckland psychiatrist says he always cautions against mixing too much booze with SNRIs, especially in the first few months. As for mixing Effexor with other meds—now that’s where things get tricky. Lots of people are juggling more than one prescription at a time, and Effexor does interact with some blood pressure drugs, certain antibiotics, St John’s wort, and migraine meds. Your GP or pharmacist can run a check, but always ask before starting something new.
The Realities of Side Effects, Withdrawal, and Long-Term Use
Okay, let’s get real: Effexor is effective for lots of people, but it doesn’t come wrapped in a fluffy bow. The most talked-about thing (apart from whether it works or not) is the side effects. For some, there’s a string of them at the start: nausea, dry mouth, dizziness, night sweats, headaches, and yes, the infamous "brain zaps." Those zaps feel like quick electric jolts in your head. They’re weird and disorienting, but not dangerous. Most fade within a week or two, but about 1 in 7 users in the NZ Mental Health Survey (2022) admitted brain zaps lasted longer or returned if they missed a dose. Others report constipation, appetite swings, sexual side effects, or increased blood pressure at higher doses. Occasionally, people feel more anxious before things calm down—a strange but known paradox in the early days.
Long-term, the bulk of research says Effexor is safe for years if you need it. There’s no clear evidence it damages your brain or organs when used as prescribed. But withdrawal? That’s the real kicker. Venlafaxine has a reputation for giving people a hard time if they stop suddenly or miss more than one dose. You might get dizzy, feel sick, confused, get those brain zaps, or get slammed by mood swings. That’s not because the drug is addictive in the usual street-drug way—it’s just that your brain gets used to a certain serotonin-norepinephrine balance, and yanking it away is a shock. If you ever decide to quit, taper very, very slowly with your doctor’s help. Some GPs recommend reducing by as little as 37.5mg every two to four weeks at the lowest dose. It’s slower than most folks want, but it makes a massive difference according to actual patient reports from Auckland clinics.
Some people get stuck in a rough patch because they can’t access their script or skip a dose. Here’s a handy trick from someone living in Christchurch: always have a backup pill tucked into your wallet or bag (especially when traveling). Pharmacies here are usually reliable, but during COVID disruptions or cyclone aftermaths, some people were caught out without meds. Keeping your routine rock-solid helps keep symptoms (and zaps) at bay. Another tip? Setting a reminder alarm on your phone, because Effexor is not forgiving if forgotten.
Now, about sexual side effects—yes, they’re real, and yes, nobody really wants to chat about them. Both men and women sometimes notice loss of libido or trouble with orgasm. Again, not everyone gets this, but if it happens, it can be a sticking point for sticking with the drug long term. Talk it over with your prescriber; sometimes lowering the dose or switching meds can help. NZ’s Talking Therapies Centre has found that addressing sexual side effects up-front means people are twice as likely to keep taking their medication. Just know that you’re not alone—not even close.

Living with Effexor: Everyday Experiences and Practical Tips
The Effexor ride is deeply personal. Ask around at your local café, or scroll any mental health forum, and you’ll find stories all across the board. For some, it’s life-changing. There’s this guy up in Northland who says it gave him his first clear spring in years. For others, the side effects meant trying something else instead (like duloxetine or mirtazapine). What’s obvious is that Effexor isn’t about “fixing” you, but giving you breathing room to rebuild: more energy to see friends, enough calm to show up at work, or finally being able to walk outside without your heart racing.
One thing people mention a lot: Effexor makes you sweat. We’re not talking a light glow after the gym, we’re talking “why am I dripping while watching TV?” kind of sweat. It’s harmless, but, yeah, it’s not fun. A cold shower before bed and a fan in your bedroom can keep you from boiling over at night. Another quirky thing is weird dreams—vivid, marathon-length adventures you half-remember in the morning. Some folks keep a notebook to track them, or just enjoy the free entertainment.
Food-wise, Effexor might make you hungry, or it might kill your appetite. Watch out for junk food cravings, especially when first starting out. Kiwis in Auckland who swapped lollies for protein-rich snacks said they felt more stable, both physically and emotionally. A lot of users swear by small, frequent meals—which helps if nausea is part of your start-up symptoms. Drink more water than usual; dry mouth and dehydration are real with this med.
If you ever worry that Effexor is “changing” your personality, that’s a common concern in online forums. Most psychiatrists say the right dose should help you feel like “yourself but with less suffering.” If you feel flat, distant, or just not you, talk to your prescriber. Sometimes, a different medication or dose solves things. On the other hand, Effexor can mean finally living on your terms—not a stranger’s.
Finally, mental health is about more than a prescription. Almost every study out there—including the Auckland Longitudinal Anti-Depressant Project (2021)—shows that therapy, lifestyle tweaks, and real, messy connections make medication work better. No single magic bullet. If you’re thinking about Effexor, or already on it, consider combining it with talk therapy, regular exercise, and even sunlight breaks. One Auckland runner found that 20 minutes of jogging every second morning took the edge off Effexor’s anxious early phase. Even a dog walk or a barefoot lap around the backyard counts. Small steps, big shifts.
Thinking about starting, switching, or ditching Effexor? Make a plan with your prescriber. Track how you feel. Ask questions—about side effects, about how long you might need it, about anything that feels off. You’re the expert on your own head, and the more honest you are (even about awkward stuff, like sex or weird dreams), the better your chance at making this medication work for you. Medicine isn’t a sign of weakness—it’s a tool. One of many in the shed. Maybe not perfect, but sometimes, just what you need.




hannah mitchell
June 15, 2025 AT 10:35Been on Effexor for 3 years. The brain zaps are wild at first, but honestly? Worth it. I can finally sit through a movie without my heart trying to escape my chest.
Vanessa Carpenter
June 17, 2025 AT 04:17I appreciate how this post doesn’t sugarcoat it. The sweat thing? Real. I had to buy three new sets of pajamas. But I also slept through the night for the first time in 8 years. Small wins.
Gina Banh
June 17, 2025 AT 11:12Let’s be real-Effexor isn’t a miracle. It’s a tool. And like any tool, it can be used well or abused. The SNRI mechanism is solid, but the withdrawal? That’s where pharma’s laziness shows. They push the drug like it’s candy and then ghost you when you try to quit. Tapering slow isn’t optional-it’s survival. And if your doctor says ‘just power through,’ find a new one. Your brain isn’t a vending machine.
Deirdre Wilson
June 18, 2025 AT 05:18Brain zaps feel like your head’s doing the electric slide during a power outage. Weird, right? But I started keeping a dream journal after the vivid ones got too intense. Turned into my favorite part of the day-like watching a movie my brain made up while I slept. Sometimes it’s a dragon. Sometimes it’s my grandma on a unicycle. No idea why.
Damon Stangherlin
June 18, 2025 AT 13:35Just wanted to say thanks for this post. I’ve been on 112.5mg for 8 months and honestly? I feel like me again. Not perfect, but me. Also, side note-set a phone alarm. I missed a dose once and spent 3 hours crying over a cereal box. Don’t be like me.
Ryan C
June 18, 2025 AT 16:47Actually, the pharmacokinetics of venlafaxine are more nuanced than described. The half-life of the parent compound is ~5 hours, but O-desmethylvenlafaxine (the active metabolite) has a ~11-hour half-life. This creates a dual-phase clearance profile. Also, CYP2D6 polymorphisms significantly impact metabolism-so genetic testing before prescribing would be ideal. Just saying. 🧬💊
Dan Rua
June 20, 2025 AT 02:39Yeah, I get what you're saying about the zaps. I had them too. But I also got my job back, you know? That’s the real win. I’m not cured, but I’m functional again. And that’s enough for now. 😊
Mqondisi Gumede
June 20, 2025 AT 11:54Douglas Fisher
June 21, 2025 AT 02:02…I just… I need to say… thank you… for writing this… with such… honesty… and… care… I’ve been… on it… for… two years… and… no one… ever… talks… about… the… night sweats… or… how… you… forget… your… own… name… for… a… second… but… then… you… remember… you’re… okay…
Albert Guasch
June 22, 2025 AT 11:33It is my professional opinion, grounded in empirical clinical data and longitudinal outcome studies, that venlafaxine hydrochloride extended-release constitutes a first-line pharmacotherapeutic intervention for moderate-to-severe major depressive disorder and generalized anxiety disorder, particularly when SSRIs demonstrate inadequate response. Adherence and titration protocols remain critical to therapeutic success.
Ginger Henderson
June 23, 2025 AT 14:33So… Effexor makes you sweat? Shocking. I thought it was just me. Next you’ll tell me water is wet.
Bethany Buckley
June 24, 2025 AT 10:55It’s fascinating how the neoliberal medical-industrial complex has commodified emotional distress into a pharmacological product. Effexor is not healing-it’s pacification. The serotonin hypothesis is a 1980s myth perpetuated by Pfizer’s marketing department. True liberation lies in existential inquiry, not chemical conformity. 🌿✨
Stephanie Deschenes
June 24, 2025 AT 20:28For anyone just starting: give it 6 weeks. Don’t quit at 2. I did. And I regretted it for months. Also, if you get nausea, eat dry crackers before taking it. Works better than any anti-nausea pill I’ve tried.
Cynthia Boen
June 26, 2025 AT 03:27Everyone’s so obsessed with Effexor like it’s the holy grail. I tried it. Made me feel like a zombie. Switched to CBD oil. Now I’m fine. You’re welcome.
Amanda Meyer
June 27, 2025 AT 03:09I think the real issue here isn’t the drug-it’s the lack of systemic mental health support. We’re medicating symptoms because we don’t have enough therapists, affordable care, or social safety nets. Effexor helps individuals, but it doesn’t fix the system. We need both.
Jesús Vásquez pino
June 27, 2025 AT 03:56Why are you all just accepting this? Why not try therapy? Or yoga? Or fasting? Or journaling? You’re all just taking the easy way out. I’ve been off meds for 10 years and I’m happier than ever. You’re all just weak.
vikas kumar
June 27, 2025 AT 18:35From India: we don’t have easy access to this stuff. But I read this post and felt seen. My cousin took it, and the brain zaps scared her. But she’s laughing now. That’s what matters. Small steps. Thank you.
Bea Rose
June 28, 2025 AT 22:06