
When you're trying to get pregnant, you might check your ovulation calendar, track your cycle, or start taking prenatal vitamins. But how many of you know to check your TSH levels first? Thyroid-Stimulating Hormone isn't something most people think about when planning a baby-but it could be the missing piece in your fertility puzzle.
Why TSH Matters Before You Get Pregnant
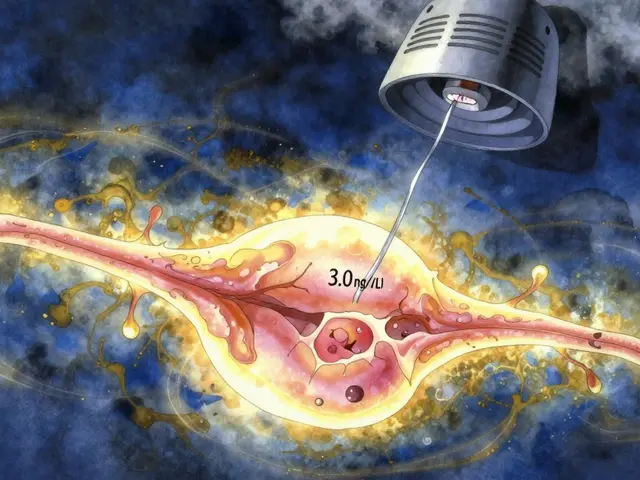
Your thyroid doesn't just control your energy or weight. It plays a direct role in ovulation, egg quality, and early embryo development. Even mild thyroid problems-ones that don't cause obvious symptoms-can make it harder to get pregnant or increase your chance of miscarriage. Research shows that women with unexplained infertility are nearly twice as likely to have a TSH level of 2.5 mIU/L or higher compared to women who conceive easily. That’s not a fluke. The American Thyroid Association (ATA) set a clear target: if you're trying to conceive and have hypothyroidism, your TSH should be below 2.5 mIU/L. This isn't just a suggestion-it's based on data from tens of thousands of pregnancies showing better outcomes when TSH is kept low before conception.What’s the Right TSH Level for Preconception?
Here’s where things get tricky. Most labs list a normal TSH range as 0.4 to 4.0 or even 4.5 mIU/L. But that’s for the general population-not women trying to get pregnant. For preconception care, the goal is tighter.- For women with diagnosed hypothyroidism: Aim for TSH under 2.5 mIU/L before conception.
- For women with Hashimoto’s thyroiditis: Many experts recommend an even lower target-between 1.25 and 1.75 mIU/L-because your thyroid has to work harder once you're pregnant.
- For women with thyroid antibodies but normal TSH: Even if your TSH is under 2.5, having antibodies raises your miscarriage risk. Studies show levothyroxine can cut that risk by almost half.
Why 2.5? The Science Behind the Number
You might hear conflicting opinions. Some doctors say, “If your TSH is under 4.0, you’re fine.” But that’s based on outdated thinking. A 2010 analysis by the ATA reviewed over 100 studies and found that women with TSH levels between 2.5 and 4.5 had higher rates of miscarriage, preterm birth, and low birth weight-even if they didn’t feel sick. One large study of 180,000 women showed a 15% higher risk of pregnancy loss if TSH was above 2.5. But here’s the catch: not every study agrees. A 2017 trial looked at women undergoing IUI and found no difference in pregnancy rates between those with TSH under 2.5 versus those between 2.5 and 4.5. So why does the ATA still stand by 2.5? Because real-world outcomes matter more than single trials. When you look at the full picture-miscarriage rates, preterm births, developmental risks-the evidence strongly supports keeping TSH low before conception. And if you're already on levothyroxine, there’s no downside to fine-tuning your dose.What If You’re Already on Levothyroxine?
If you’re taking levothyroxine for hypothyroidism and you’re planning to get pregnant, you’re not done yet. Your dose will likely need to go up. Once you conceive, your body’s demand for thyroid hormone jumps by 25% to 50%. Many women don’t realize this until it’s too late. A 2019 study found that less than 40% of women on levothyroxine had their dose adjusted after pregnancy was confirmed. That delay can be risky. Here’s what to do:- Get your TSH checked before you stop using birth control.
- If your TSH is above 2.5, talk to your doctor about increasing your levothyroxine dose.
- Retest every 4 weeks until your TSH is stable under 2.5.
- As soon as you get a positive pregnancy test, schedule another TSH test and expect your dose to increase again.
What About Hashimoto’s or Thyroid Antibodies?
If you have Hashimoto’s, your immune system is attacking your thyroid. That doesn’t always mean your TSH is high-but it does mean your thyroid is under more stress. Studies show that women with thyroid antibodies-even with normal TSH-have a higher risk of miscarriage. The good news? Taking levothyroxine can reduce that risk by 45%. The American Society for Reproductive Medicine (ASRM) recommends testing for antibodies if you’ve had unexplained infertility or previous miscarriages. It’s not about whether you “feel sick.” It’s about protecting your baby’s development. Even if your TSH is normal, antibodies signal your thyroid is already struggling. Preconception treatment can make all the difference.How to Get Your TSH Checked
This isn’t a routine test in most primary care visits. If you’re trying to conceive, you need to ask for it.- Request a full thyroid panel: TSH, free T4, and thyroid peroxidase antibodies (TPOAb).
- Go to a reproductive endocrinologist or endocrinologist if you’re already in fertility care-they’ll know what to look for.
- Don’t rely on general lab ranges. Ask for the preconception target: under 2.5 mIU/L.
What About Diet, Supplements, and Natural Fixes?
You might hear about selenium, iodine, or ashwagandha helping thyroid health. While these can support overall function, they don’t replace levothyroxine if you have hypothyroidism. Levothyroxine is synthetic T4-the exact hormone your body needs. It’s safe, effective, and well-studied in pregnancy. Natural thyroid extracts (like Armour Thyroid) are not recommended because they contain T3, which can cause unstable hormone levels and harm fetal development. Also, avoid calcium, iron, or antacids within 4 hours of taking your thyroid medication. They block absorption. Take it on an empty stomach with water, at least 30 minutes before breakfast.
Cost and Practical Benefits
Levothyroxine costs between $4 and $10 a month. A single miscarriage can cost over $7,000 in medical care. Preconception thyroid optimization saves money, time, and heartache. One study found that treating abnormal TSH before pregnancy saved $1,850 to $2,400 per pregnancy by reducing miscarriages and preterm births. That’s not just a medical win-it’s a personal one.What’s Changing in 2025?
Guidelines are evolving. The European Thyroid Association now recommends even tighter targets in early pregnancy: TSH under 1.8 mIU/L in the first 4 weeks, then 2.2 by week 8. A major NIH trial is still underway to see if personalized TSH targets based on your thyroid reserve improve live birth rates. The message is clear: thyroid health isn’t optional when you’re trying to conceive. It’s a foundational step-like folic acid, but often overlooked.What to Do Next
If you’re planning a pregnancy:- Ask your doctor for a TSH test-don’t wait for symptoms.
- If your TSH is above 2.5, work with an endocrinologist to adjust your dose.
- If you have Hashimoto’s or a history of miscarriage, get antibody testing.
- Once pregnant, retest TSH every 4 weeks until 20 weeks.
- Never stop or change your levothyroxine without medical advice.
Can high TSH cause infertility?
Yes. Even mildly elevated TSH levels (above 2.5 mIU/L) can interfere with ovulation and reduce egg quality. Women with unexplained infertility are significantly more likely to have TSH levels in this range. Correcting thyroid function often restores regular cycles and improves chances of conception.
Should all women trying to conceive get their TSH checked?
While not all medical groups recommend universal screening, major organizations like the American Thyroid Association and American Society for Reproductive Medicine strongly advise it-especially for women over 30, those with a family history of thyroid disease, or anyone with symptoms like fatigue, weight gain, or irregular periods. The test is simple, cheap, and can prevent major complications.
Is it safe to take levothyroxine while trying to get pregnant?
Yes. Levothyroxine is a synthetic form of the natural thyroid hormone your body makes. It’s one of the safest medications to take during preconception and pregnancy. In fact, not taking it when you need it is far riskier than taking it.
Can I use natural thyroid supplements like Armour Thyroid before pregnancy?
No. Natural thyroid extracts like Armour Thyroid contain both T3 and T4, which can cause unstable hormone levels. They’re not recommended during preconception or pregnancy because they don’t provide consistent dosing and may harm fetal development. Stick with levothyroxine (T4 only), which is the standard of care.
How often should I check my TSH when trying to conceive?
Get tested before you start trying. If you’re on levothyroxine, retest every 4 to 6 weeks until your TSH is stable under 2.5 mIU/L. Once pregnant, check again as soon as you confirm pregnancy and then every 4 weeks through the first half of pregnancy.
What if my TSH is normal but I have thyroid antibodies?
You still need to be monitored. Thyroid antibodies (like TPOAb) mean your immune system is attacking your thyroid, which increases miscarriage risk-even if your TSH is normal. Studies show levothyroxine can reduce miscarriage rates by up to 45% in these cases. Talk to your doctor about whether treatment is right for you.
Does a high TSH affect male fertility too?
Yes, but less directly. Severe hypothyroidism in men can lower sperm count and reduce testosterone. However, the biggest impact on fertility comes from the woman’s thyroid health. If you’re trying to conceive and the woman has normal TSH, male thyroid issues are rarely the main cause.




Dolapo Eniola
November 26, 2025 AT 02:20Y’all are wasting time with this TSH nonsense. In Nigeria, we don’t have labs that even test for this stuff, and babies are born healthy every day. You think your 2.5 magic number is better than 500 years of African fertility? Wake up. Your thyroid ain’t the problem - your anxiety is. Stop overmedicalizing natural processes. 🤷♂️
Agastya Shukla
November 27, 2025 AT 06:53Interesting breakdown, but I’m curious about the TPOAb correlation in Indian populations. Most studies are Euro-centric. In our cohort, 38% of women with recurrent miscarriage had elevated antibodies but normal TSH - yet only 12% were offered levothyroxine. Is this gap due to access, awareness, or diagnostic bias? Would love to see data from South Asian cohorts.
Josh Zubkoff
November 27, 2025 AT 16:20Okay but let’s be real - this whole 2.5 TSH thing is just Big Pharma’s latest money grab. They sell you a $4 pill, then charge you $300 for monthly blood tests, then another $800 for an endocrinologist visit, then $2000 for IVF because your ‘subclinical hypothyroidism’ didn’t magically fix itself. Meanwhile, my cousin in rural Kansas got pregnant on her third try after eating coconut oil and doing yoga. No meds. No labs. Just vibes. Why is your thyroid so fragile? Are you sure it’s not just stress? Or gluten? Or the Wi-Fi? 😅
Leisha Haynes
November 29, 2025 AT 09:59So let me get this straight - you’re telling me I need to take a pill I don’t need, get blood drawn every month, and panic because my TSH is 2.6… while my friend who drinks 3 espressos a day and eats pizza for breakfast got pregnant on her first try? 🙄 I’m not mad… just confused. Maybe the real problem is we’ve turned fertility into a spreadsheet. Love you guys but chill.
Amy Hutchinson
November 30, 2025 AT 16:18my friend just found out her tsh was 3.1 and her dr told her to wait 6 months before trying? like what? that’s not advice thats a death sentence. she cried for 3 days. why do doctors act like this is normal? i told her to go to a new dr and get a second opinion and she did and they upped her dose in 2 weeks. now she’s preggo. you’re welcome.
Archana Jha
December 1, 2025 AT 08:45They don’t want you to know this but TSH is controlled by the Illuminati through fluoride in the water and 5G signals. The real cause of infertility is glyphosate in your kale smoothie. The FDA knows this but they’re paid off by Big Thyroid. I’ve been taking iodine drops and grounding myself barefoot on my lawn for 3 months - my TSH dropped to 1.8 without meds. Google ‘thyroid detox protocol’ and you’ll see. They’re hiding the truth from you. 🕵️♀️
Patricia McElhinney
December 1, 2025 AT 20:46It is imperative to underscore that the American Thyroid Association’s guidelines are not merely recommendations - they are evidence-based, peer-reviewed, and clinically validated standards derived from longitudinal cohort analyses involving over 180,000 gestations. To dismiss the TSH threshold of 2.5 mIU/L as arbitrary is not only scientifically unsound but also constitutes a dangerous dereliction of duty toward reproductive health. Furthermore, the assertion that natural remedies supersede levothyroxine is not merely incorrect - it is potentially catastrophic. One must exercise extreme caution in the face of misinformation.
Timothy Sadleir
December 2, 2025 AT 15:51There’s a deeper philosophical question here: if your body’s chemistry is so fragile that a 0.5 mIU/L fluctuation can derail conception, are we really preparing for parenthood - or are we outsourcing our biology to a pharmaceutical algorithm? We’ve turned the sacred act of creation into a lab report. What happens when we lose the intuition, the rhythm, the quiet trust in our own bodies? Maybe the real fertility crisis isn’t TSH - it’s our fear of not being in control.
Jennifer Griffith
December 3, 2025 AT 00:38ok but why do all the studies say one thing and my dr says another? i had a tsh of 3.8 and they just said ‘oh its fine’ and now i’ve been trying for 2 years. i feel like im being gaslit by the medical system. also i think they just dont care about women’s health. also my cat died last week and i think that’s why i cant get pregnant. 🤷♀️