
Omega-3 Dosage Calculator for Diabetic Neuropathy
Recommended Daily Omega-3 Intake
Omega-3 Sources for Diabetic Neuropathy
Key Takeaways
- Omega-3 fatty acids can reduce inflammation and protect nerve cells in diabetic peripheral neuropathy (DPN).
- EPA and DHA are the two most studied omega-3s for nerve health; EPA leans toward anti‑inflammatory action, DHA supports membrane repair.
- Clinical trials show modest pain relief (10‑30% reduction) when patients supplement with 1-3g of combined EPA/DHA daily.
- Best sources include fatty fish, fortified foods, and high‑quality algae or fish‑oil capsules.
- Start with a low dose, monitor blood sugar, and talk to a healthcare provider before adding omega‑3s to your regimen.
When you hear the term Omega-3 Fatty Acids is a family of polyunsaturated fats that includes eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), the first thought is often heart health. Yet a growing body of research ties these fats to nerve protection, especially for people living with diabetes who struggle with peripheral neuropathy.
What Is Diabetic Peripheral Neuropathy?
Diabetic peripheral neuropathy (DPN) is a nerve‑damage condition that affects up to 50% of long‑standing diabetics. It typically starts in the feet and hands, causing tingling, burning, or sharp shooting pains. The damage stems from chronic high blood glucose, which triggers oxidative stress, inflammation, and microvascular injury. Over time, the myelin sheath- the protective coating around nerves- thins, slowing signal transmission and creating the classic “glove‑and‑sock” sensation.
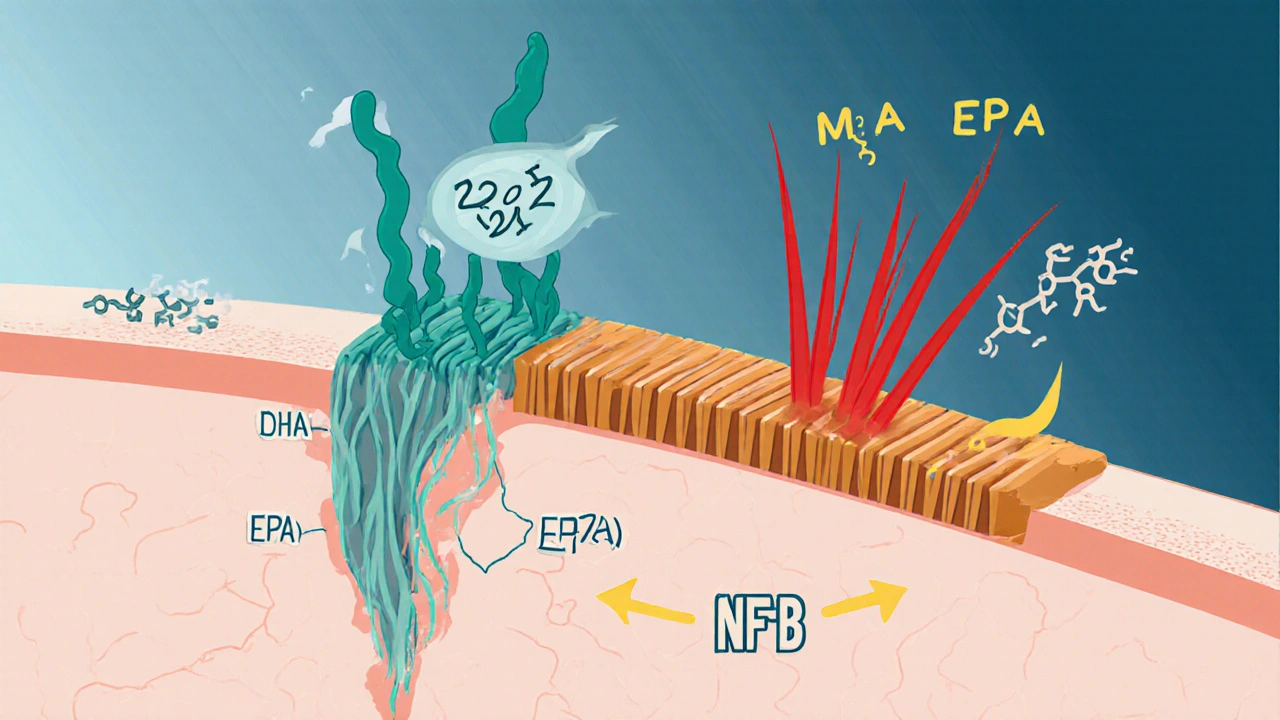
Patients often ask why some diabetics develop severe pain while others hardly notice any symptoms. Genetics, blood‑sugar control, and lifestyle factors all play a role, but the underlying biochemical cascade is remarkably similar: excess glucose leads to advanced glycation end‑products (AGEs), which amplify free‑radical production and activate inflammatory pathways such as NF‑κB.
Omega-3 Fatty Acids: The Basics
EPA (eicosapentaenoic acid) and DHA (docosahexaenoic acid) are the two long‑chain omega‑3s most linked to nerve health. EPA primarily suppresses the production of pro‑inflammatory eicosanoids, while DHA integrates into neuronal membranes, improving fluidity and supporting the growth of new synaptic connections.
Dietary sources are straightforward: wild‑caught salmon, mackerel, sardines, and trout deliver 1-2g of combined EPA/DHA per 100g serving. For vegetarians, algae‑derived supplements provide the same DHA profile, and some fortified eggs or dairy products contain modest amounts.
How Omega-3s Influence Nerve Health
The link between omega‑3s and DPN hinges on three biological actions:
- Anti‑inflammatory effect: EPA competes with arachidonic acid for the cyclooxygenase (COX) enzyme, shifting eicosanoid production toward less inflammatory series (e.g., prostaglandin E3). This dampens the NF‑κB cascade that fuels nerve‑cell injury.
- Membrane repair: DHA’s 22‑carbon chain fits neatly into phospholipid bilayers, restoring the flexibility of myelin sheaths. Better membrane dynamics help nerves fire more efficiently and resist oxidative damage.
- Neurotrophic support: Both EPA and DHA up‑regulate brain‑derived neurotrophic factor (BDNF) and nerve growth factor (NGF). These proteins encourage axonal sprouting and protect against apoptosis.
Put together, these mechanisms translate into fewer pain signals and a slower progression of sensory loss.
What the Evidence Says
Multiple randomized controlled trials (RCTs) have examined omega‑3 supplementation in diabetic neuropathy. Below is a snapshot of three pivotal studies:
- Study A (2021, 120 participants): 2g EPA+DHA daily for 24weeks reduced the Neuropathy Pain Scale by 22% versus placebo, with no change in HbA1c.
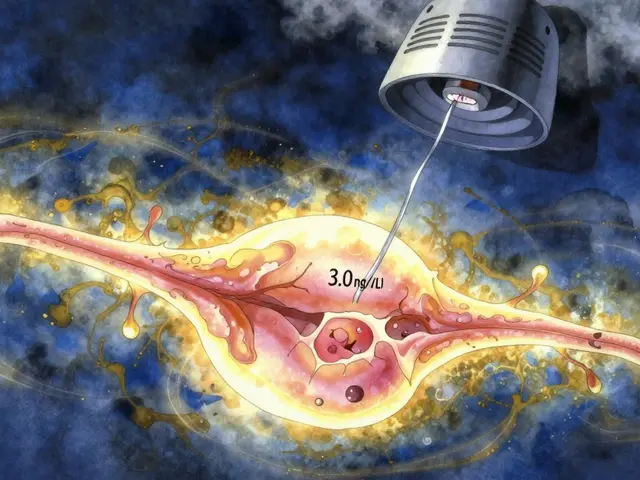
- Study B (2023, 80 participants): High‑purity DHA alone (1.5g) improved nerve conduction velocity by 0.4m/s after 12weeks, a modest but statistically significant gain.
- Study C (2024, meta‑analysis of 9 RCTs): Average pain reduction across studies was 15% (range 10‑30%). Sub‑analysis showed greater benefits when baseline vitamin D levels were sufficient, hinting at synergistic effects.
While results are encouraging, researchers note that omega‑3s are not a cure; they work best as an adjunct to glucose control, exercise, and approved neuropathy medications.
Practical Guidance for Adding Omega-3s
| Attribute | EPA | DHA |
|---|---|---|
| Primary action | Reduces inflammatory eicosanoids | Enhances membrane fluidity |
| Typical dose for DPN | 1-2g/day | 0.5-1.5g/day |
| Best food source | Cold‑water fish (mackerel, sardines) | Fatty fish (salmon) or algae oil |
| Research focus | Pain intensity reduction | Improved nerve conduction |
For most adults, a combined EPA/DHA dose of 1-3g daily is safe and effective. Start with 500mg per day, split between meals, and gradually increase if tolerated. Choose certified, molecular‑distilled fish‑oil capsules to minimize oxidation and contaminants like mercury.
Incorporating whole foods is equally important. Aim for two servings of fatty fish per week, or a daily serving of algae‑based smoothies if you avoid animal products. Pair omega‑3s with a balanced diet rich in antioxidants (berries, leafy greens) to further combat oxidative stress.
Potential Risks and Interactions
Omega‑3s are generally well‑tolerated, but a few cautions apply:
- Bleeding risk: High doses (>5g) may thin blood; patients on anticoagulants (warfarin, clopidogrel) should discuss dosage with their doctor.
- Blood sugar changes: Some evidence hints at a slight improvement in insulin sensitivity, but sudden large increases could affect glucose monitoring.
- GI upset: Burping or fishy aftertaste is common; enteric‑coated capsules can help.
Always review supplement labels for added vitamins (e.g., vitamin E) that could amplify antioxidant effects but also increase bleed‑risk when combined with prescription drugs.
Putting It All Together
Managing diabetic peripheral neuropathy is a multi‑pronged effort. Tight glycemic control remains the cornerstone, but adding omega-3 fatty acids offers a scientifically backed way to ease pain, protect nerve structure, and possibly slow disease progression. The key is consistency-daily intake for at least three months is needed before noticeable improvement.
If you’re curious about trying omega‑3s, follow these steps:
- Check your blood sugar and medication list with your clinician.
- Choose a reputable EPA/DHA supplement (≥300mg EPA and ≥200mg DHA per capsule).
- Start with 1 capsule per day for two weeks, then increase to 2‑3 capsules as tolerated.
- Track pain scores and any side effects in a simple journal.
- Re‑evaluate with your healthcare team after 12 weeks to decide on continuation.
When combined with regular exercise, foot care, and a diet low in refined carbs, omega‑3s can become a valuable ally in the fight against diabetic nerve pain.
Frequently Asked Questions
Can omega‑3 supplements replace my prescription neuropathy meds?
No. Omega‑3s work best as a complementary approach. They may lower the dose needed for some drugs, but you should never stop a prescribed medication without your doctor’s advice.
How long before I feel any pain relief?
Most studies report noticeable changes after 8-12 weeks of consistent dosing. Individual response varies, so patience and regular monitoring are important.
Is fish oil safe if I have high triglycerides?
Yes. In fact, EPA/DHA can lower triglyceride levels. Still, keep your cardiologist in the loop, especially if you’re on lipid‑lowering drugs.
What’s the difference between regular fish oil and “pharmaceutical‑grade” omega‑3?
Pharmaceutical‑grade products undergo stricter purification, guaranteeing higher EPA/DHA concentrations (often >90%) and lower oxidation. They’re more expensive but provide a consistent dose.
Do I need to take a vitamin D supplement alongside omega‑3?
Vitamin D deficiency can blunt nerve‑protective effects. If your levels are low, a combined regimen may be beneficial, but test first.




Jesús Vásquez pino
October 4, 2025 AT 14:53hannah mitchell
October 6, 2025 AT 12:08stephen riyo
October 7, 2025 AT 10:42Jaspreet Kaur
October 9, 2025 AT 05:27Gina Banh
October 9, 2025 AT 19:34Bethany Buckley
October 11, 2025 AT 16:41Stephanie Deschenes
October 12, 2025 AT 05:51Cynthia Boen
October 14, 2025 AT 00:44Amanda Meyer
October 15, 2025 AT 16:21Albert Guasch
October 16, 2025 AT 20:30Ginger Henderson
October 18, 2025 AT 00:44vikas kumar
October 18, 2025 AT 00:53Bea Rose
October 19, 2025 AT 01:18Michael Collier
October 20, 2025 AT 10:01Shannon Amos
October 20, 2025 AT 15:49Wendy Edwards
October 22, 2025 AT 01:36Deirdre Wilson
October 23, 2025 AT 18:43Damon Stangherlin
October 25, 2025 AT 07:36Ryan C
October 26, 2025 AT 23:06