BPH and Bladder Stone Risk Assessment Tool
How Your Habits Affect Risk
The article explains that urinary retention from enlarged prostate creates conditions where minerals can crystallize into stones. This tool estimates your risk based on key factors.
Enter your values above to see your risk level
Key Takeaways
- Enlarged prostate (BPH) can trap urine, creating a breeding ground for stone formation.
- Bladder stones often cause the same painful symptoms as a blocked prostate, so doctors look for both.
- Imaging tests such as ultrasound and CT pinpoint the size and location of stones and the prostate.
- Medications that relax the prostate muscle or shrink its tissue reduce stone risk.
- Staying hydrated, a balanced diet, and regular check‑ups keep both problems at bay.
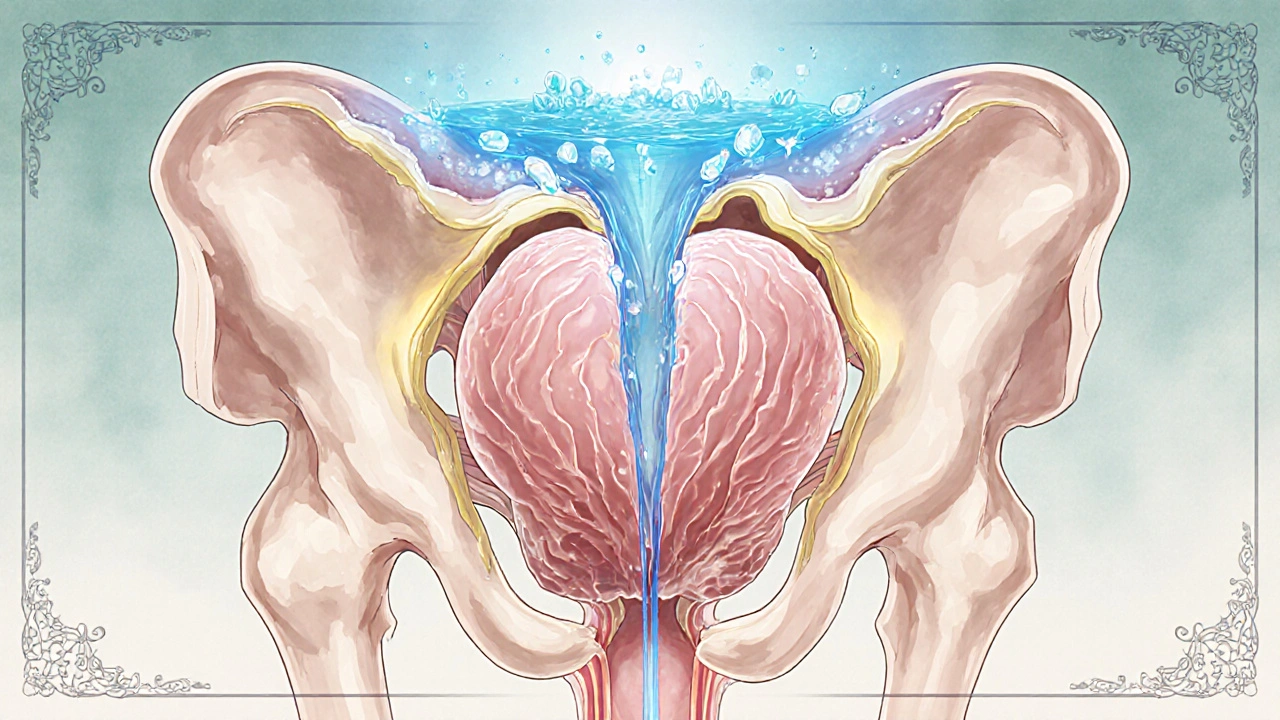
When men start noticing an urgent need to pee, a weak stream, or a feeling that the bladder never fully empties, they usually think about an enlarged prostate is a condition where the gland around the urethra grows bigger, often called benign prostatic hyperplasia (BPH). What’s less obvious is that this blockage can also set the stage for bladder stones are hard mineral deposits that form inside the bladder when urine sits stagnant for too long.
What Is an Enlarged Prostate?
The prostate sits just below the bladder and surrounds the urethra. As men age, the gland’s cells multiply, leading to a gradual increase in size. This growth, medically known as Benign prostatic hyperplasia (BPH), is not cancerous, but it can compress the urethra and limit urine flow.
Key symptoms (collectively called lower urinary tract symptoms or Lower urinary tract symptoms (LUTS)) include:
- Frequent daytime urination
- Nocturia - waking up several times at night
- Weak or interrupted stream
- Sudden urge to empty the bladder
- Feeling of incomplete emptying
These signs arise because the enlarged gland creates urinary retention, where urine pools in the bladder after each void.
What Are Bladder Stones?
Bladder stones, also called vesical calculi, develop when minerals such as calcium oxalate, uric acid, or struvite crystallize and clump together inside the bladder. They can range from a grain of sand to several centimeters.
Typical causes include:
- Chronic urinary retention (urine stays still long enough to crystallize)
- Infections that raise the pH of urine, favoring stone growth
- Bladder outlet obstruction - the very same blockage caused by an enlarged prostate
- Foreign bodies or catheters left in the bladder
Symptoms often mimic those of BPH: painful urination, blood in the urine, and a persistent urge to pee, which is why doctors frequently investigate both conditions together.
How an Enlarged Prostate Triggers Bladder Stones
The link is straightforward: an obstructed urethra stops urine from draining completely, leaving a residual volume in the bladder. When urine sits, several processes happen simultaneously:
- Concentration rise: Solutes become more concentrated, encouraging crystal nucleation.
- pH shift: Stagnant urine often becomes more alkaline, especially if bacteria produce urease, leading to struvite stone formation.
- Infection risk: Residual urine serves as a breeding ground for bacteria, which further alter urine chemistry.
Over weeks or months, tiny crystals grow into visible stones that can aggravate the blockage, creating a vicious cycle.
Symptoms Overlap - Why Misdiagnosis Happens
Both BPH and bladder stones share the same warning signs, so a patient might be treated for “just an enlarged prostate” while the real culprit is a stone lodged near the bladder neck. Distinguishing features include:
- Hematuria (blood in urine) is more common with stones.
- Painful urination tends to be sharper with stones, often described as a “gravel‑like” sensation.
- Intermittent obstruction - patients with stones may notice sudden relief after passing a fragment, a pattern not typical of pure BPH.
Because the overlap is so close, clinicians rely on imaging and lab tests to separate them.
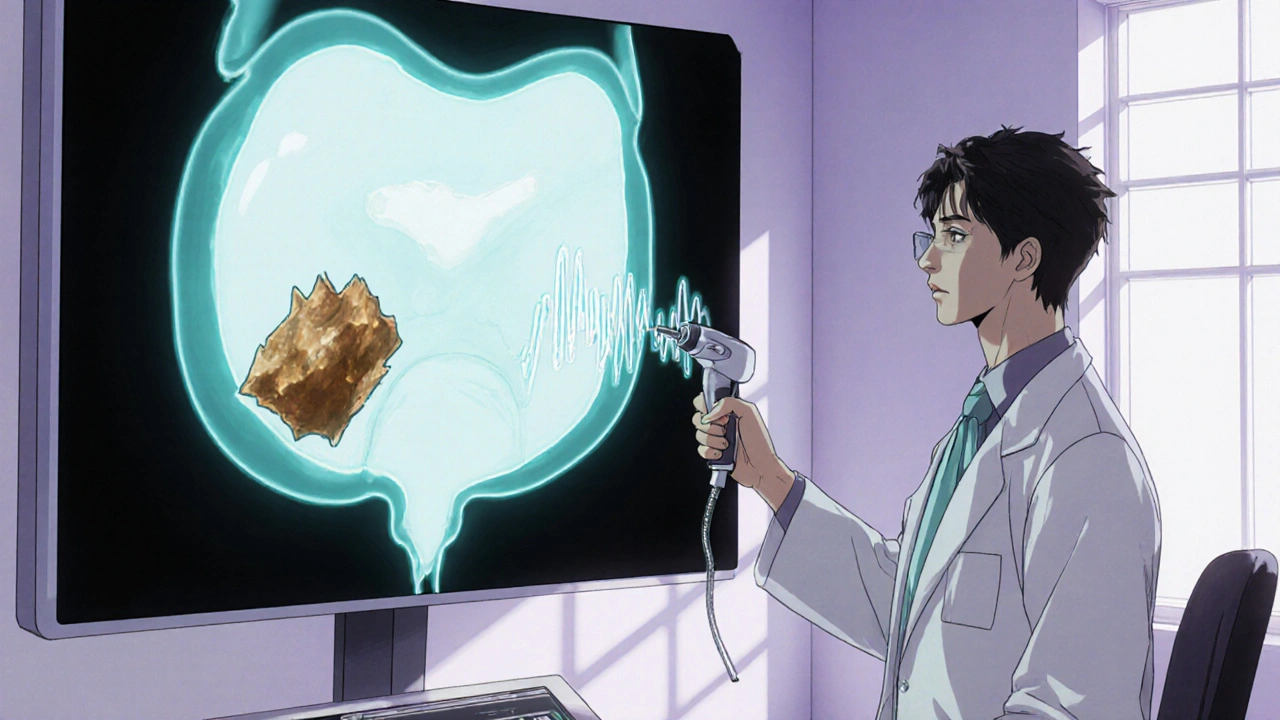
Diagnostic Tools
When a doctor suspects both conditions, they usually order a combination of the following:
- Digital rectal exam (DRE) - feels the prostate size and consistency.
- Prostate‑specific antigen (PSA) blood test - helps rule out cancer, though it isn’t definitive for BPH.
- Ultrasound - a quick, non‑invasive way to see the prostate’s volume and detect stones.
- CT scan or plain X‑ray (KUB) - provides detailed images of calcifications, especially useful for larger stones.
- Cystoscopy - a thin camera inserted through the urethra to directly view the bladder interior; the gold standard for confirming stone location.
Once the size of the prostate and any stones are known, treatment can be tailored.
Treatment Options for an Enlarged Prostate
Therapy aims to relieve obstruction and, indirectly, reduce stone formation. The main approaches are:
- Alpha blockers (e.g., tamsulosin, alfuzosin) - relax smooth muscle in the prostate and bladder neck, improving urine flow.
- 5‑alpha‑reductase inhibitors (e.g., finasteride, dutasteride) - shrink prostate tissue over several months by blocking hormone conversion.
- Combination therapy - using both drug classes for faster symptom relief.
- Minimally invasive procedures:
- Transurethral resection of the prostate (TURP) - a surgeon removes part of the gland through the urethra.
- Laser enucleation - uses laser energy to vaporize excess prostate tissue.
- UroLift - small implants lift and hold the prostate open without cutting tissue.
For men where medication fails or the prostate is very large, surgery provides the most reliable relief and simultaneously clears the path for stone removal.
Managing and Removing Bladder Stones
Stone treatment depends on size, composition, and symptom severity:
- Small stones (under 5 mm) may pass spontaneously with increased fluid intake.
- Endoscopic removal - a cystoscope is used to break the stone with laser or grasp it with forceps.
- Extracorporeal shock wave lithotripsy (ESWL) - sound waves break larger stones into fragments that can be expelled.
- Open surgery - rare, reserved for extremely large or multiple stones.
Antibiotics are prescribed if an infection is present, and dietary adjustments (reducing oxalate‑rich foods, limiting animal protein) help prevent recurrence.
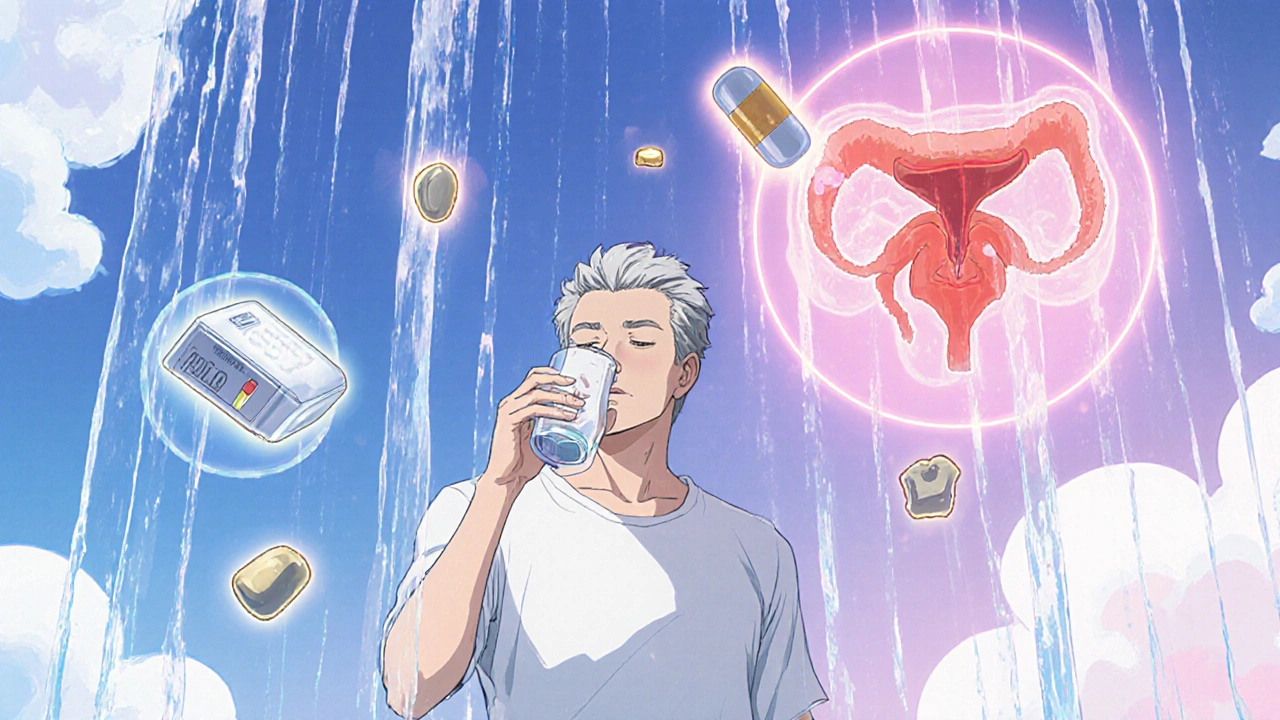
Preventive Strategies - Keeping Both Problems Away
Because the two conditions feed off each other, a combined prevention plan works best:
- Stay hydrated - aim for at least 2‑3 liters of water daily to dilute urine.
- Timed voiding - go to the bathroom every 3‑4 hours, even if you don’t feel a full bladder.
- Limit caffeine and alcohol - both irritate the bladder and increase urgency.
- Balanced diet - plenty of fruits, vegetables, and whole grains; avoid excessive salt, which raises calcium excretion.
- Regular check‑ups - an annual prostate exam and urine analysis catch early changes.
- Medication adherence - if prescribed alpha blockers or 5‑alpha‑reductase inhibitors, take them consistently to keep the prostate size in check.
Implementing these habits reduces residual urine, lowers infection risk, and keeps stone‑forming minerals from concentrating.
Living With BPH and Bladder Stones
Most men will experience some urinary changes as they age. Knowing that an enlarged prostate can lead to bladder stones empowers you to act early. If you notice sudden blood in the urine, severe pain, or a dramatic change in flow, seek medical attention promptly - early intervention prevents larger stones and more invasive surgeries.
Frequently Asked Questions
Can an enlarged prostate cause bladder stones?
Yes. When the prostate blocks urine flow, residual urine stays in the bladder, creating a high‑concentration environment where minerals can crystallize into stones.
What are the first signs that I might have bladder stones?
Blood in the urine, a gritty feeling during urination, frequent urges, and lower‑abdominal pain are common early clues.
Do medications for BPH also prevent stones?
Alpha blockers improve urine flow, lowering the chance of urine stasis, which indirectly reduces stone risk. However, they don’t dissolve existing stones.
Is surgery always required for bladder stones?
No. Small stones often pass with increased fluid intake. Larger stones usually need endoscopic removal or lithotripsy, while very large stones may need open surgery.
How often should I get screened for prostate problems?
Men over 50 should have an annual digital rectal exam and discuss PSA testing with their doctor. If you have urinary symptoms, schedule a visit earlier.
Understanding the connection between an enlarged prostate and bladder stones lets you spot warning signs early, choose the right tests, and adopt preventive habits that keep both conditions in check.




parbat parbatzapada
October 21, 2025 AT 03:26Been reading this and it's kinda scary how a simple gland can turn into a nightmare. The idea that urine just sits there, like a secret poison pool, feels like a plot they don't tell you about. I keep wondering if the doctors are hiding something in those scans. Maybe the whole system is designed to keep us in the hidn. Anyway, staying hydrated might be the only weapon we have.
Eryn Wells
October 21, 2025 AT 05:40Thanks for sharing this clear breakdown! 🙌 It’s great to see how staying hydrated and regular check‑ups can make a huge difference. I encourage everyone to talk openly about these issues – no shame in caring for our health. 😊 Keep the info coming!
Kathrynne Krause
October 21, 2025 AT 07:36Understanding the cascade from prostate enlargement to stone formation is nothing short of a biological symphony, each instrument playing a crucial role in the overall health of the urinary system. First, the enlarged gland creates a bottleneck that slows the outflow of urine, allowing it to linger and concentrate solutes that would otherwise be flushed away. This lingering fluid becomes a fertile breeding ground for mineral crystals, much like a stagnant pond invites algae to bloom. As the concentration of calcium, oxalate, and uric acid climbs, nucleation sites appear, sparking the birth of microscopic stone embryos. Over time, these embryos coalesce, growing layer by layer until they are large enough to cause pain and obstruction. The presence of a stone then exacerbates the blockage, creating a vicious feedback loop that amplifies both symptoms and complications. Moreover, the altered pH environment in retained urine often tips toward alkalinity, favoring the formation of struvite stones in the presence of urease‑producing bacteria. These bacteria not only change the chemical landscape but also provoke inflammation, further irritating the bladder wall. Patients may experience a gritty sensation during voiding, hematuria, and sudden urgency that mimics a simple prostate issue but actually signals stone activity. Imaging modalities such as ultrasound and CT scans act as detectives, revealing both the swollen prostate and any hidden calculi lurking behind it. Therapeutically, alpha blockers relax the smooth muscle at the bladder neck, improving flow and reducing stasis, while 5‑alpha‑reductase inhibitors gradually shrink the prostate tissue itself. When medication falls short, minimally invasive procedures like TURP or laser enucleation remove the obstruction, simultaneously restoring proper drainage and facilitating stone clearance. Endoscopic laser lithotripsy can then pulverize remaining stones into passable fragments, sparing patients from open surgery. Lifestyle modifications-ample water intake, balanced diets low in oxalates, and timed voiding-serve as the frontline defense, preventing the initial cascade from ever igniting. Regular follow‑ups with a urologist ensure that any subtle changes are caught early, before they evolve into full‑blown stones. In sum, a proactive, integrated approach that tackles both prostate enlargement and stone risk is the most effective strategy for preserving urinary health.
Erika Thonn
October 21, 2025 AT 09:50One can ponder the silent dialogue between a swollen gland and the liquid that pools within, as if the body whispers warnings we ignore. The stone, a humble crystal, emerges from this quiet tension, embodying the paradox of stillness birthing disruption. Yet, our modern rush to silence such signs leaves the patient adrift in a sea of discomfort. Perhaps the true cure lies not only in pills but in listening to the inner cadenace of our own excretory rhythm. If we attune ourselves, the bladder may speak clearer and the prostate may calm. This thought, though simple, tempts the mind to reflect on health as philosophy.
Jake Hayes
October 21, 2025 AT 12:20Your summary misses the critical point: BPH alone seldom causes stones without urinary stasis. Medications must be optimized before considering invasive procedures. Skipping proper imaging is negligent. Follow evidence‑based protocols.
Brandy Eichberger
October 21, 2025 AT 14:33Permit me to commend the thoroughness of this exposition; such comprehensive overviews are a rarity in popular discourse. The integration of pathophysiology with pragmatic management reflects a commendable scholarly balance. While the tone remains accessible, the underlying nuance respects the reader's intellect. I encourage continued dissemination of this caliber of medical literacy. Warm regards to all contributors.
Eli Soler Caralt
October 21, 2025 AT 16:46The interplay of anatomy and chemistry in this context evokes a silent opera, each note resonating within the hidden chambers of our uro‑system. 😐 One must contemplate the stoic patiences required of the bladder as it endures prolonged restraint. Yet, the modern aversion to introspection leaves many unaware of the subtle cues preceding stone formation. 🧐 In my humble view, embracing both scientific rigor and reflective mindfulness offers the most elegant path forward. 🌿
John Price
October 21, 2025 AT 18:43Hydration is key, so drink up.