
Linezolid Tyramine Intake Calculator
Tyramine Calculator
Calculate your total tyramine intake while on linezolid. The safe limit is 100mg per day.
When prescribing Linezolid an oxazolidinone‑class antibiotic that also inhibits monoamine oxidase enzymes, clinicians must think about more than just the infection. The drug’s weak but real MAO‑inhibiting effect can turn a harmless cheese plate into a blood‑pressure emergency if patients eat foods rich in Tyramine a naturally occurring amine found in aged, fermented, or spoiled foods. This guide breaks down the science, the real‑world cases, and the steps you can take to keep patients safe while they finish their course.
Why Linezolid Acts like a mild MAO inhibitor
Linezolid was designed to block bacterial protein synthesis, but studies from the University of Toronto showed it also blocks both MAO‑A and MAO‑B by about 40‑50 % at therapeutic levels (600 mg twice daily). That degree of inhibition is enough to let tyramine slip past the usual “filter” and cause a surge of norepinephrine, which spikes blood pressure. Unlike classic irreversible MAO inhibitors, linezolid’s effect wears off in 24‑48 hours after stopping the drug, but during treatment the interaction is clinically significant.
How tyramine triggers hypertension
Under normal circumstances, MAO enzymes break down tyramine before it reaches the bloodstream. When MAO activity is blocked, tyramine is absorbed, releases stored catecholamines, and can push systolic pressure above 180 mmHg in minutes. The British Journal of Clinical Pharmacology trial reported a tyramine sensitivity factor of 1.8 for linezolid, meaning patients were almost twice as likely to react compared with placebo. Body‑mass index also mattered-higher BMI linked to larger spikes, so patient‑specific factors matter.
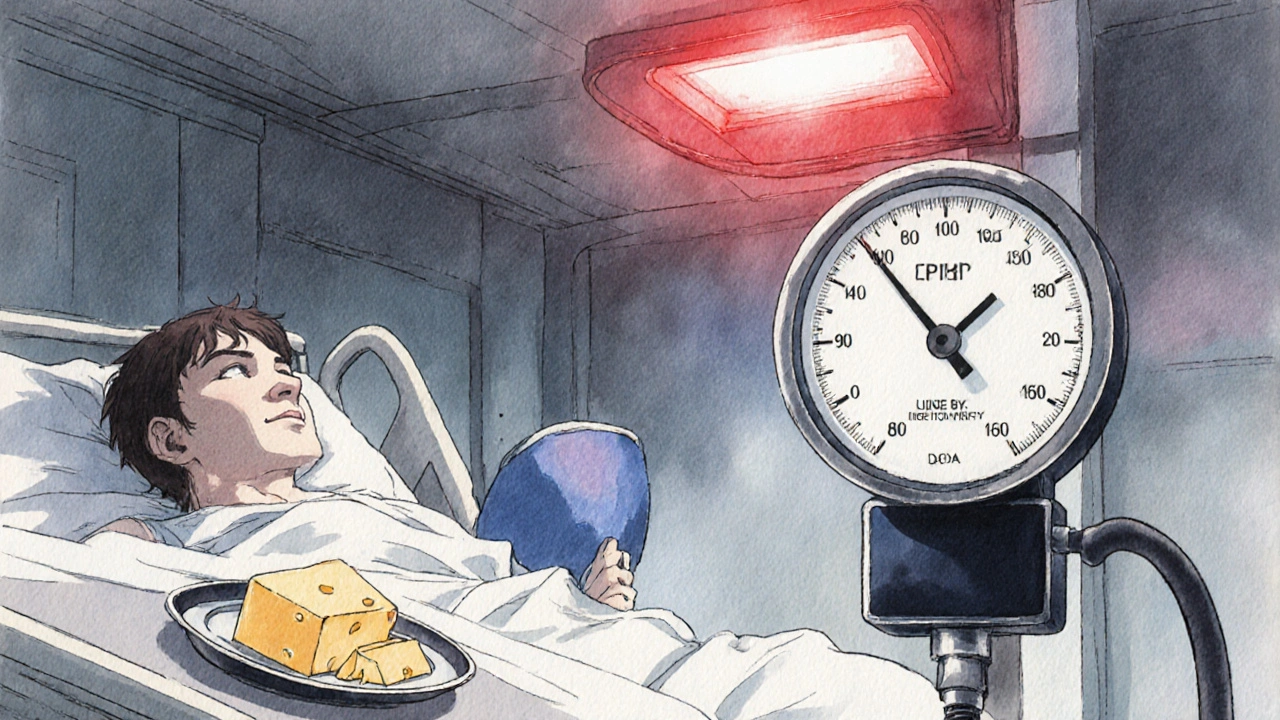
Real‑world evidence of hypertensive crises
Case reports are sobering. A 2021 Journal of Antimicrobial Chemotherapy series described 17 linezolid‑related hypertensive crises over five years; the average systolic reading hit 212 mmHg, and 65 % needed ICU care. One patient ate aged cheddar (≈150 mg tyramine) while on linezolid and presented with 230/130 mmHg, requiring three days in the ICU. Conversely, a small handful of PatientsLikeMe users say they tolerated moderate tyramine without issue, but those anecdotes lack verification and likely under‑represent milder events.
Which foods carry the most tyramine?
Guidelines set a 100 mg threshold per day. Below is a quick reference of common culprits and the approximate tyramine per typical serving:
| Food | Typical serving | Tyramine (mg) |
|---|---|---|
| Aged cheddar | 1 oz (28 g) | 150‑300 |
| Blue cheese | 1 oz | 900‑1500 |
| Tap beer | 12 oz | 120‑200 |
| Red wine | 5 oz | 30‑100 |
| Fermented soy (miso, natto) | 1 tbsp | 60‑120 |
| Salami, pepperoni | 2 oz | 80‑150 |
| Improperly stored fish | 4 oz | 200‑400 |
These numbers help clinicians give concrete advice: “One slice of aged cheddar equals roughly 150 mg tyramine-stay under the 100 mg daily limit.”
Other drug interactions to watch
Linezolid’s MAO inhibition also amplifies serotonergic agents (SSRIs, SNRIs, tramadol), raising the specter of serotonin syndrome. Sympathomimetics like pseudoephedrine or decongestants can add to the pressor effect. Dopaminergic drugs (e.g., levodopa) have also caused severe spikes. The safest route is to pause or substitute these meds while the patient is on linezolid, or at least monitor blood pressure closely.
Practical steps for clinicians
- Baseline assessment: Check blood pressure before starting linezolid, especially in hypertensive patients.
- Patient education: Provide a one‑page handout with a food list, served at the pharmacy or bedside. Visual aids work better than a verbal disclaimer.
- Dietary timing: Begin restrictions 24 hours before the first dose and continue for 14 days after the last dose, matching the 5‑day MAO‑recovery half‑life.
- Monitoring: For high‑risk patients, measure BP twice daily during therapy; for low‑risk, check every 48 hours.
- Medication review: Temporarily stop serotonergic or sympathomimetic drugs, or substitute them with non‑MAO‑interacting alternatives.
- Documentation: Record the restriction in the electronic health record and set an alert for discharge instructions.
Studies show that when institutions use electronic alerts and dietitian consults, compliance jumps from 44 % to over 80 %.
Future outlook: antibiotics without MAO inhibition
New agents like contezolid (MRX‑I) are in Phase III trials and promise the same gram‑positive coverage without MAO‑related risks. If approved, they could replace linezolid for outpatient therapy, reducing the need for dietary counseling. Until then, the linezolid tyramine interaction remains a real safety concern that must be managed.
Quick reference checklist
- Avoid foods >100 mg tyramine per day (aged cheeses, tap beer, fermented soy, aged meats).
- Screen for serotonergic or sympathomimetic meds.
- Check baseline BP; re‑check twice daily if hypertensive.
- Start dietary restrictions 24 h before first dose.
- Continue restrictions 14 days after last dose.
- Document and provide written handout.
- Consider dietitian referral for prolonged courses.
Can I have a glass of wine while on linezolid?
Red wine can contain up to 100 mg tyramine per 5‑oz glass. Because the safe limit is 100 mg per day, even one glass could push you over the threshold. The safest advice is to avoid wine for the duration of therapy and two weeks after.
What if I forget a dietary restriction?
If a high‑tyramine meal is unintentionally eaten, monitor blood pressure every hour for the next 4‑6 hours. If systolic pressure climbs above 160 mmHg, contact a provider; an oral antihypertensive (e.g., nifedipine) may be needed.
Do I need to stop my SSRI while on linezolid?
Because both linezolid and SSRIs raise serotonin, the combination can trigger serotonin syndrome. Either stop the SSRI (if possible) or choose a non‑serotonergic antidepressant. Consult the prescribing physician before making changes.
How long does the MAO‑inhibition last after stopping linezolid?
MAO activity typically recovers within 24‑48 hours after the last dose, but guidelines advise continuing tyramine restriction for 14 days to be safe for slower recoverers.
Are there any over‑the‑counter meds I should avoid?
Pseudoephedrine (found in many cold remedies) and phenylephrine can add to blood‑pressure spikes. Choose a non‑decongestant alternative like chlorpheniramine, and always check the label.



Grace Silver
October 24, 2025 AT 21:30Linezolid’s hidden MAO twist really puts diet on the doctor’s radar.
Clinton Papenfus
November 3, 2025 AT 02:43Clinicians must incorporate dietary counseling into the prescribing workflow; the evidence for tyramine‑induced hypertension is compelling and the risk is quantifiable. A concise handout detailing foods that exceed 100 mg of tyramine per day can serve as a practical tool. Baseline blood pressure measurement before initiation is advisable, especially in patients with pre‑existing hypertension. Ongoing monitoring during therapy completes the safety net.
Zaria Williams
November 14, 2025 AT 16:30The tyramine issue with linezolid isn’t just a textbook footnote, it’s a daily reality for many patients.
When you block MAO‑A and MAO‑B even partially, the gut‑brain axis gets a free pass for dietary amines.
That means a simple snack of aged cheddar can balloon norepinephrine levels in a matter of minutes.
In practice I’ve seen the BP surge from 130/80 to 220/130 while the patient was still chewing their cheese.
The emergency team had to pump IV nicardipine just to get the numbers back under control.
What’s scary is that the same reaction can happen with fermented soy, tap beer, or even a mis‑stored piece of fish.
The literature shows a tyramine sensitivity factor of 1.8, but real‑world cases suggest it could be higher in obese or older folks.
You also have to remember that linezolid’s MAO inhibition fades only after 24‑48 hours, so the diet restriction must linger past the last dose.
A practical tip is to give patients a one‑page handout that lists foods >100 mg per serving and a simple “no” sign for anything aged.
Pair that with a baseline BP check and a follow‑up reading every 48 hours for low‑risk, twice daily for high‑risk patients.
If a patient accidentally eats a high‑tyramine meal, watch their systolic pressure every hour for at least six hours.
Should it climb above 160 mmHg, an oral nifedipine 10 mg can be prescribed as a rescue.
Also keep an eye on serotonergic meds because the combo can tip into serotonin syndrome.
In my clinic we switched a patient off an SSRI before starting linezolid and avoided a nasty interaction.
Finally, educate the whole care team – nurses, pharmacists, and dietitians – because the burden shouldn’t fall on the patient alone.
When everyone knows the red flags, the hypertensive crises become rare events instead of headline cases.
ram kumar
November 26, 2025 AT 06:17Ah, the melodrama of a cheese‑induced hypertensive episode – truly the Shakespeare of modern pharmacology. One would think prescribing an antibiotic would be straightforward, yet we are forced to become culinary gatekeepers. The patient’s misstep becomes a tragic tableau, blood pressure soaring as if the heavens themselves were offended. Such theatrics demand a more elegant solution than endless pamphlets.
Melanie Vargas
December 7, 2025 AT 20:03Great points, everyone! 😊 Let’s keep the conversation supportive – sharing handout templates and reminder apps can really help patients stay on track. 🍽️📋
Deborah Galloway
December 19, 2025 AT 09:50I’ve seen the impact of clear communication first‑hand. When we gave patients a simple “no cheese” card, adherence jumped and we avoided two ICU admissions in a month. It’s amazing how a tiny visual cue can make such a big difference.
Charlie Stillwell
December 30, 2025 AT 23:37Seriously, this is just another excuse to over‑complicate a straightforward antibiotic course. Stop feeding the hype – use the drug, monitor BP, and move on. 🤖
Ken Dany Poquiz Bocanegra
January 11, 2026 AT 13:23Keep it simple: baseline BP, avoid high‑tyramine foods, and check numbers regularly.
Tamara Schäfer
January 23, 2026 AT 03:10Ths post rvlates a crutial ptnt saftey isue – whn linezold blk MAOenzmes, even smal amt of tyrmine cn triger a spkshoot bet pressur.
Patients often not kno the hidden tyramine in everyday foods – like a simple pizza sauce or aged salami.
We shld give them a clear list, not a long wall of text. A bright‑colord chart works best.
Also, remind them to hold off on over‑the‑counter decongestants – they can add to the pressur spike.
Finally, set a reminder in the EMR to re‑check blood pressure 48 hours after finishing linezolid – the MAO effect can linger.
Tamara Tioran-Harrison
February 3, 2026 AT 16:57Oh, splendid – another “must‑read” pamphlet that will probably gather dust on a pharmacy shelf. 🙄 Perhaps we should also issue a royal decree for patients to abstain from breathing entirely while on linezolid. 🤦♀️
kevin burton
February 6, 2026 AT 20:30In summary, a multidisciplinary approach-physicians, pharmacists, dietitians-combined with straightforward patient education and routine blood‑pressure monitoring effectively mitigates the linezolid‑tyramine risk.