
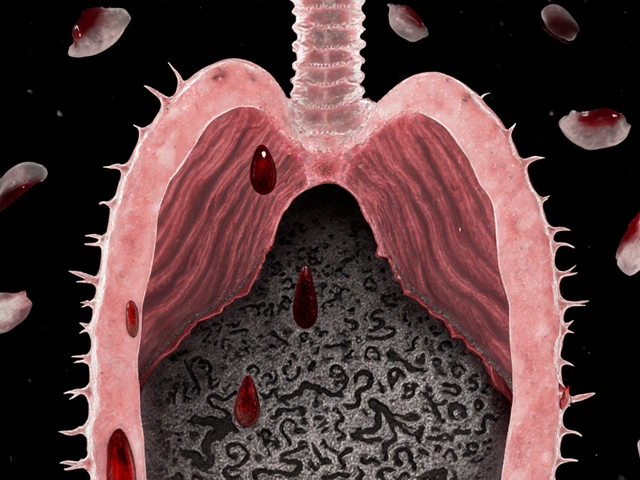
Most people with asthma or COPD rely on inhalers to control their symptoms. But here’s the hard truth: if you’re not using your inhaler right, you’re getting maybe 10% of the medicine you paid for. That’s not a typo. Up to 90% of users mess up the technique, and it’s not because they’re careless-it’s because no one ever showed them how to do it properly.
Why Your Inhaler Isn’t Working Like It Should
Metered-dose inhalers (MDIs) are tiny, handheld devices that spray medicine into your lungs. They’ve been around since the 1950s, but the way they work hasn’t changed much. The medicine comes out in a quick burst-lasting less than a fifth of a second. If you don’t time your breath right, most of it hits your tongue, throat, or the back of your mouth. That’s not just wasteful. It’s dangerous. When medicine doesn’t reach your lungs, you’re more likely to have flare-ups, end up in the ER, or need stronger doses. Studies show that improper use leads to 50% of preventable asthma hospitalizations in the U.S. alone. And here’s the kicker: 80% of the medicine ends up stuck in your mouth and throat when you use it wrong. That’s why steroid inhalers cause thrush in 5-10% of users-it’s not the drug, it’s the technique.The 8-Step Correct Inhaler Technique
This isn’t guesswork. It’s science-backed, step-by-step, and works for all HFA-based inhalers like Ventolin HFA, Flovent HFA, Advair HFA, and Symbicort. Do this every single time.- Remove the cap and check that nothing’s blocking the mouthpiece. Shake the inhaler for 5-10 seconds. (Some, like Alvesco and QVAR, don’t need shaking-check your label.)
- Exhale fully-empty your lungs completely. Don’t just breathe out a little. Blow out like you’re trying to fog up a mirror from across the room.
- Hold the inhaler upright with your thumb on the bottom and your index finger on top. Place the mouthpiece between your teeth and seal your lips tightly around it. Don’t hold it an inch away-that’s for old CFC inhalers. This is the #1 mistake.
- Start breathing in slowly just before or at the exact moment you press down. Don’t wait. Don’t inhale too fast. Aim for a slow, steady breath over 3-5 seconds. You want to feel the medicine moving down, not spraying in your mouth.
- Press the inhaler once to release the dose. Keep breathing in slowly after you press. Don’t rush it.
- Hold your breath for 10 seconds. This is non-negotiable. Studies show holding your breath for 10 seconds increases lung delivery by 30%. Count it out: “One-Mississippi, Two-Mississippi…”
- Exhale slowly through your nose. Don’t cough or blow hard right after.
- Rinse your mouth with water and spit it out. This is critical if you’re using a steroid inhaler. It cuts the risk of oral thrush by 40%.
Common Mistakes (And How to Fix Them)
Most people think they’re doing it right. They’ve used the inhaler for years. But here’s what’s really happening:- Pressing too late - 68% of users press the inhaler after they’ve already started breathing in. Result? Medicine hits the throat. Fix: Start inhaling just before you press. Practice with a placebo inhaler.
- Not exhaling first - 42% skip this step. Your lungs are full of air, so the medicine can’t go deep. Fix: Always empty your lungs completely before inhaling.
- Breathing too fast - 57% inhale too hard and too quick. The medicine particles are 50-150 microns. If you inhale faster than 30 liters per minute, they bounce off your airways. Fix: Practice slow, steady breaths. Imagine sipping hot tea through a straw.
- Skipping the breath hold - 63% exhale immediately. You’re losing 30% of the dose. Fix: Set a 10-second timer on your phone. Do it until it becomes automatic.
- Not priming - 31% don’t prime new or unused inhalers. A new canister might deliver only half the dose if not primed. Prime with 2-4 sprays into the air (check your brand’s instructions).

Spacers: The Secret Weapon You’re Not Using
If you’re struggling with timing, a spacer is your best friend. It’s a plastic tube that attaches to your inhaler. You spray the medicine into the spacer, then breathe in slowly from it. No need to coordinate the press with your breath. Studies show spacers boost lung delivery from 10-20% to 70-80%. They’re especially helpful for kids, older adults, and anyone with shaky hands. A 2022 study found patients using spacers had 45% fewer asthma attacks than those using inhalers alone. You don’t need a prescription. Most pharmacies sell them for under $15. Look for one with a mask if you’re using it for a child. Clean it weekly with soapy water and let it air dry. Never wipe it with a towel-it creates static that traps medicine.When to Switch to a Different Inhaler
Not everyone should use an MDI. If you can’t inhale slowly, or your breath is too weak (less than 30 liters per minute), an MDI won’t work well. In that case, consider:- Dry Powder Inhalers (DPIs) - like Advair Diskus or Symbicort Turbuhaler. You inhale fast and hard-no timing needed. But if you can’t take a deep, quick breath, they won’t work.
- Soft Mist Inhalers - like Respimat. They release a slow, fine mist over 1.5 seconds. No spacer needed. Good for people who struggle with coordination.

What to Do If You’re Still Struggling
You’re not alone. On Reddit’s asthma community, 78% of users said they didn’t get it right until they had a hospital visit. Here’s what to do next:- Ask your doctor or pharmacist to watch you use your inhaler-right now. Don’t just say “I know how.” Show them. Most won’t ask unless you bring it up.
- Use a placebo inhaler for practice. These are empty versions that make the same click sound. Practice the steps without wasting medicine.
- Watch a video from the American Lung Association or your inhaler’s manufacturer. Many now include QR codes on the box that link to official technique videos.
- Try a smart inhaler - devices like Propeller or Adherium track your use and give feedback via an app. They’re 92% accurate at spotting technique errors.
Long-Term Wins: Why This Matters
Getting this right isn’t just about avoiding side effects. It’s about living better. People who use their inhalers correctly:- Use their rescue inhaler 35% less often
- Have fewer emergency visits
- Need lower doses of medication
- Save money-$3.20 for every $1 spent on proper training
How do I know if my inhaler is empty?
Most inhalers have a counter that shows how many doses are left. If yours doesn’t, track how many you’ve used. A standard inhaler has 120 or 200 puffs. Divide that by how many times you use it per day. For example, if you use it twice a day, a 120-puff inhaler lasts 60 days. Don’t rely on how it feels-shaking it or spraying it into the air won’t tell you if it’s empty. When the counter hits zero, replace it.
Can I use my inhaler without shaking it?
Some inhalers, like Alvesco and QVAR, don’t need shaking because their medicine is already evenly mixed. But most, including Ventolin HFA, Flovent HFA, and Advair HFA, require shaking for 5-10 seconds. Skipping this step can reduce your dose by up to 40%. Always check the label or ask your pharmacist.
Why does my inhaler sometimes taste bitter or cause a sore throat?
That’s medicine sticking in your mouth and throat, not reaching your lungs. It’s a sign your technique is off. Make sure you’re exhaling fully before inhaling, sealing your lips around the mouthpiece, and holding your breath for 10 seconds. Rinsing your mouth with water after each use also helps wash away leftover medicine and prevents thrush.
Is it okay to use my inhaler more than prescribed?
If you’re using your rescue inhaler more than twice a week (not counting exercise), your asthma isn’t under control. Overusing it can mask worsening symptoms and lead to serious complications. Talk to your doctor. You may need a different controller medication or better technique. Never exceed the maximum daily dose listed on the label.
Can children use inhalers correctly?
Most children under 6 can’t coordinate the hand-breath timing needed for an MDI. That’s why spacers with masks are recommended for kids. The mask fits over the nose and mouth, and the child takes 5-6 slow breaths after the inhaler is sprayed. Parents report 63% better results with spacers than with inhalers alone. Always supervise your child’s use.



Cara C
December 21, 2025 AT 09:15I used to think I was doing it right until my ER visit last year. Turns out I wasn’t holding my breath at all. Now I set a 10-second timer on my phone every time I use my inhaler. It’s weird at first but now it’s automatic. My lungs feel better and I’m not coughing as much. Seriously, just try it.
Also, spacers are a game changer. I got one for $12 at CVS and it’s the best money I’ve ever spent on my asthma.
Michael Ochieng
December 23, 2025 AT 00:17As someone who’s lived in three countries and used five different inhalers, let me tell you-this guide is spot on. In Nigeria, I saw people using inhalers like they were spray deodorant. No shaking, no breath hold, no rinse. It’s insane. I started handing out printed copies of this to my cousins back home. One of them went from 3 ER trips a year to zero. Just show people how to do it. Simple. Human. Effective.
Grace Rehman
December 23, 2025 AT 15:29So let me get this straight-we’ve had inhalers since the 50s and the only thing that’s changed is the propellant and the price tag
And yet we still expect people to magically know how to use them like some kind of ancient ritual
Meanwhile the pharmaceutical companies are making bank off the 90% who mess it up and then sell them more meds to fix the problems they caused
And we wonder why healthcare is broken
Also I just learned I’ve been pronouncing ‘metered-dose’ wrong this whole time
oops
Jerry Peterson
December 23, 2025 AT 21:57My dad’s COPD got way better after he started using a spacer. He’s 72, arthritic hands, can’t coordinate anything anymore. The spacer let him breathe without stress. We got one with a mask so he doesn’t even have to hold it-just put it on his face and breathe. He calls it his ‘magic tube.’
Pharmacies should give these out free with every prescription. It’s not a luxury. It’s part of the treatment.
Meina Taiwo
December 23, 2025 AT 22:00Always rinse after steroid inhalers. Always. Thrush is painful and preventable.
Southern NH Pagan Pride
December 25, 2025 AT 18:30Did you know the FDA approved inhalers in 1956 but never required proper training because the Big Pharma lobby wanted people to keep buying more
Also the 10 second breath hold? That’s from a 1989 study funded by GlaxoSmithKline
And the spacer studies? All funded by the same companies that sell spacers
They want you to think you’re doing it right so you don’t question why you’re still wheezing
And why do they call it ‘HFA’? Hydrofluoroalkane? Or is it a code for something else
Also my neighbor says the inhaler has a microchip now
maybe they’re tracking us
Orlando Marquez Jr
December 26, 2025 AT 21:16It is imperative to underscore the clinical significance of proper inhaler technique, as delineated in the preceding exposition. The efficacy of pharmacologic intervention is demonstrably contingent upon the fidelity of patient adherence to the prescribed methodology. Suboptimal delivery mechanisms not only compromise therapeutic outcomes but also contribute to the escalation of healthcare expenditures and increased morbidity. It is therefore recommended that clinicians institute standardized demonstration protocols during every encounter involving inhaler prescription. Furthermore, the utilization of spacer devices should be considered a first-line adjunctive intervention in populations exhibiting diminished inspiratory flow rates or neuromuscular coordination deficits. The evidence base supporting these interventions is robust and warrants universal implementation.
Jackie Be
December 28, 2025 AT 08:38I used to use my inhaler like a spray can and thought I was fine until I passed out at work
Then I watched the video on the box and cried because I realized I’d been doing it wrong for 12 years
Now I do the 8 steps every time like a prayer
And I rinse like my life depends on it
Because it does
Spacers are my soulmates
My lungs are thanking me
And I’m not scared to breathe anymore
Thank you whoever wrote this
YOU SAVED ME