Chronic acid reflux isn’t just a nuisance. For some people, it’s a slow-burning fuse leading to esophageal cancer. If you’ve had heartburn for five years or more - even if it’s mild - you’re not just dealing with discomfort. You’re at risk for a dangerous transformation inside your esophagus. The good news? You can spot the warning signs early and stop it before it turns deadly.
GERD Isn’t Just Heartburn - It’s a Precancerous Signal
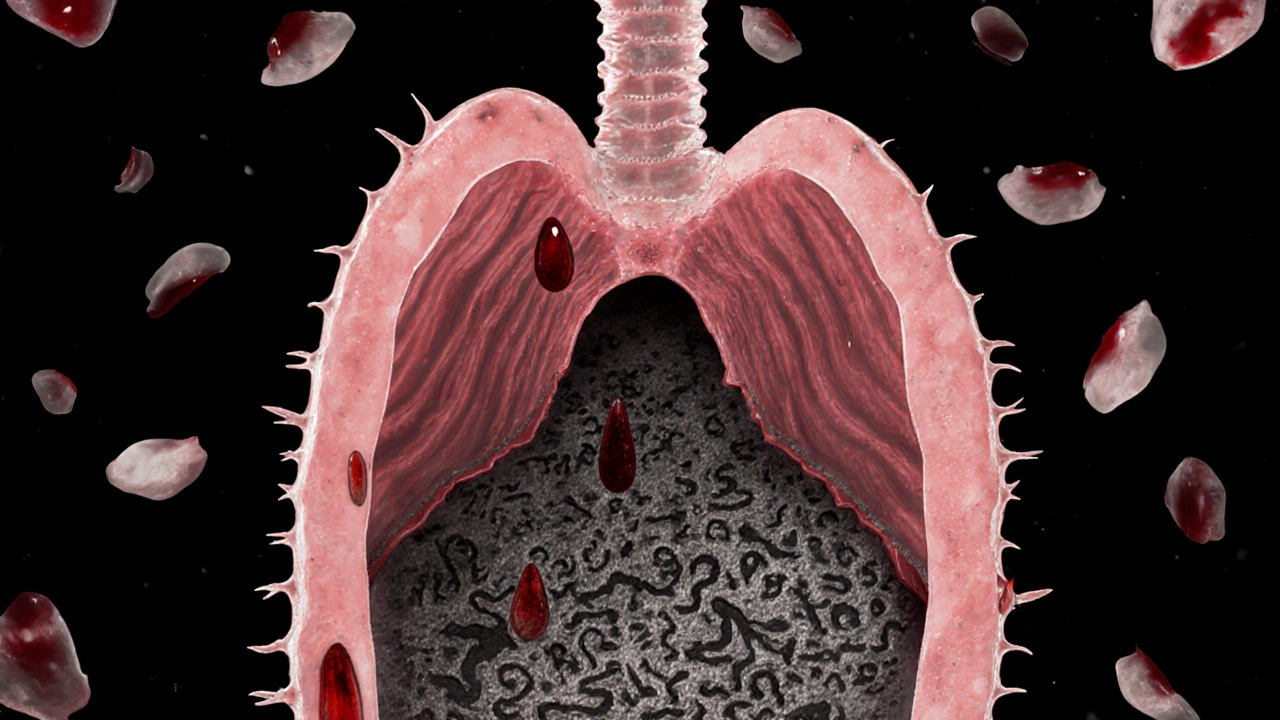
Most people think of GERD as occasional heartburn after spicy food or late-night meals. But when it happens two or more times a week for five years or longer, it’s not just inconvenient. It’s a medical red flag. The constant backflow of stomach acid damages the delicate lining of your esophagus. Over time, your body tries to protect itself by replacing the normal cells with ones that look more like stomach lining. This change is called Barrett’s esophagus - the only known precursor to esophageal adenocarcinoma, the most common type of esophageal cancer in the U.S.Here’s the hard truth: about 20% of Americans have GERD. But only 0.5% to 2% of those people develop Barrett’s esophagus. And of those, only 0.2% to 0.5% per year turn into cancer. Sounds low? But because so many people have GERD, that small percentage adds up. In 2023, over 21,000 new cases of esophageal cancer were diagnosed in the U.S. alone, and nearly 17,000 people died from it. Most of those cases were caught too late.
What makes GERD so dangerous is how silent the progression is. You might feel fine. You might even be taking medication. But the damage is still happening. A 2023 NIH study found that people with long-term GERD had a 3.2 times higher risk of esophageal cancer compared to those without it. And if your symptoms hit weekly? That risk jumps to 7 times higher.
Who’s Really at Risk? It’s Not Just Anyone With Heartburn
Not everyone with GERD will get cancer. But certain people are far more vulnerable. The risk isn’t random - it’s predictable. If you’re a white male over 50, with a BMI over 30, who smokes or used to smoke, and you’ve had acid reflux for over 10 years, your risk is significantly higher. In fact, this group makes up the majority of cases.Men are three to four times more likely than women to develop this cancer. Age matters too - 90% of cases happen after 55. Obesity plays a huge role: extra weight increases pressure on your stomach, forcing acid upward. Studies show that losing just 5-10% of your body weight cuts GERD symptoms by 40%. Smoking? It doubles or triples your risk. And if you have a family history of esophageal cancer, your odds go up even more.
Race also plays a role. White non-Hispanic Americans have three times the rate of adenocarcinoma compared to Black Americans. Why? It’s not fully understood, but genetics, diet, and access to care may all contribute. The key takeaway? If you fit even two or three of these risk factors - and you’ve had GERD for five years or more - you’re in the high-risk group. That’s not a guess. It’s what the American College of Gastroenterology recommends screening for.
The Red Flags No One Talks About (But Should)
Most people wait until they’re in serious pain before seeing a doctor. But esophageal cancer rarely hurts at first. The real warning signs are subtle - and often ignored.- Dysphagia - Feeling like food gets stuck in your chest or throat. This happens in 80% of cases at diagnosis. At first, it’s just solids. Later, even liquids become hard to swallow.
- Unexplained weight loss - Losing more than 10 pounds in six months without trying. Your body is telling you something’s wrong.
- Chronic hoarseness or cough - If you’ve had a raspy voice or persistent cough for more than two weeks, especially if you have GERD, it could be acid irritating your vocal cords.
- Food impaction - Food getting stuck so badly you have to stop eating or even go to the ER.
- New or worsening reflux after age 50 - If you never had heartburn before, but now you’re having it regularly after turning 50, especially with other risk factors, get checked.
These aren’t just ‘maybe’ symptoms. They’re the ones doctors see in nearly every patient diagnosed with late-stage cancer. And here’s the kicker: 75% of esophageal cancers are found at stage three or four - when treatment options are limited and survival rates drop below 20%. Early detection can double your chances of survival.
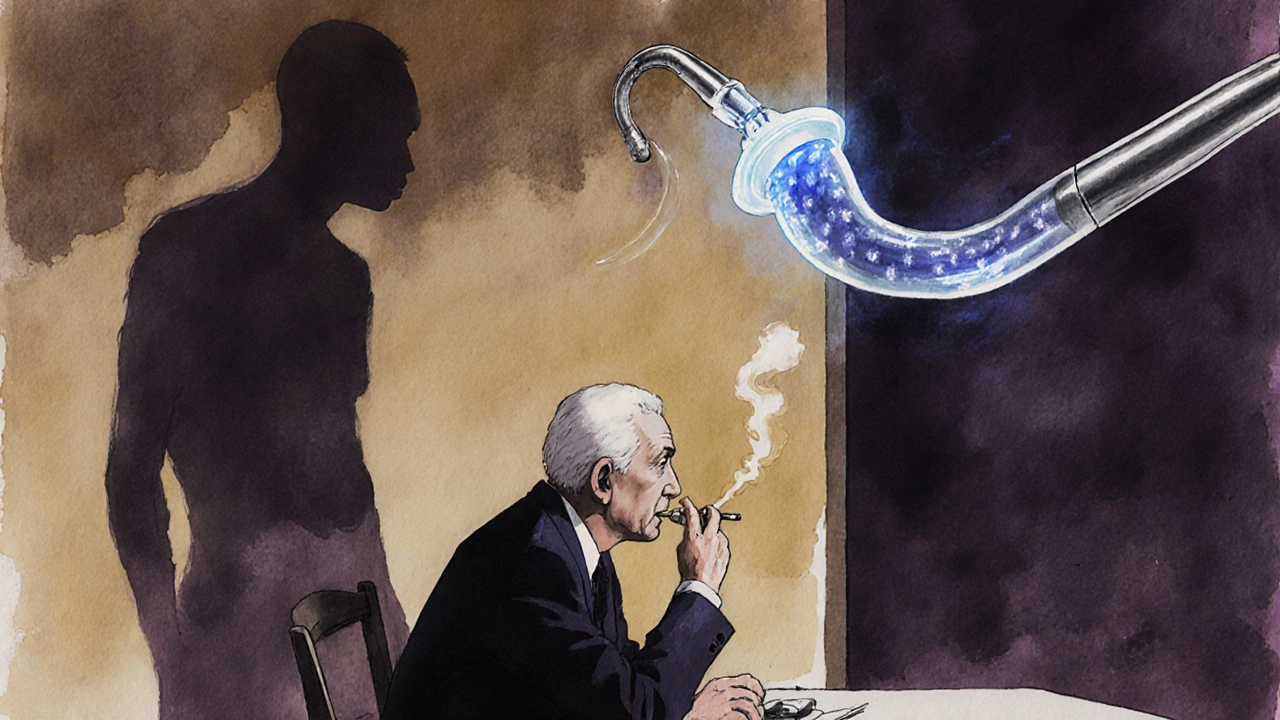
What Doctors Recommend - And Why Most People Skip It
The American College of Gastroenterology says white men over 50 with chronic GERD (five+ years) and two other risk factors - like obesity, smoking, or family history - should get an upper endoscopy. That’s a simple, quick procedure where a thin camera is passed down your throat to look for Barrett’s esophagus.But here’s the problem: only 13% of high-risk people actually get screened. Why? Many think, ‘I’m on medication, so I’m fine.’ Or, ‘It’s not that bad.’ Or, ‘I don’t have time.’ But medications like PPIs (proton pump inhibitors) only reduce acid - they don’t reverse the cellular changes already made. Only an endoscopy can see them.
And if Barrett’s is found? That’s not the end. It’s the beginning of prevention. Regular monitoring - every 3 to 5 years - can catch precancerous changes early. When dysplasia (abnormal cell growth) is caught and removed during endoscopy, cancer mortality drops by 60-70%. That’s not a small win. That’s life-saving.
What You Can Do Right Now to Lower Your Risk
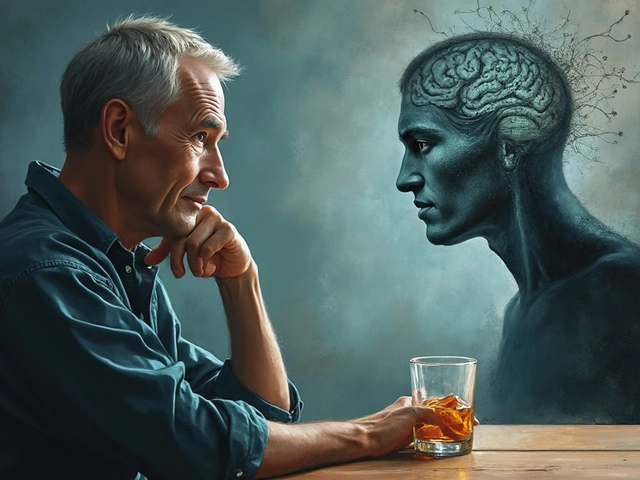
You don’t have to wait for symptoms to get worse. You can act today.- Quit smoking. Within 10 years of quitting, your cancer risk drops by half.
- Lose weight. Even a 5-10% drop in body weight cuts GERD symptoms by 40%.
- Limit alcohol. More than two drinks a day for men (or one for women) increases squamous cell cancer risk. Stick to moderation.
- Treat GERD properly. Don’t just take antacids when you feel bad. If you’re on PPIs, take them consistently. A 2023 study showed that taking PPIs for five+ years cuts cancer risk by 70% in people with Barrett’s esophagus.
- Ask for an endoscopy. If you’re over 50, male, white, overweight, a smoker, and have had GERD for five+ years - don’t wait. Ask your doctor for a screening.
There’s also exciting new tech on the horizon. A pill-sized sponge called Cytosponge, which you swallow and then pull back up, collects cells from your esophagus. It’s less invasive than endoscopy and found Barrett’s esophagus with nearly 80% accuracy in a 2022 Lancet study. It’s not everywhere yet - but it’s coming.

The Bigger Picture: Why This Is Getting Worse
Since 1975, esophageal adenocarcinoma has increased by 850%. Why? Because our diets, lifestyles, and waistlines have changed. Obesity rates have more than doubled. GERD is more common than ever. And we’re not screening enough. We treat the symptoms - the heartburn - but we ignore the silent progression underneath.But here’s the hopeful part: we know how to stop it. We know who’s at risk. We know what to look for. We have tools to catch it early. The gap isn’t in science - it’s in action. If you’re in a high-risk group, don’t assume you’re safe because you’re not in pain. Don’t wait for the red flags to turn into emergency rooms. Talk to your doctor. Get screened. Take control before it’s too late.
Can GERD cause cancer even if I take medication?
Yes. Medications like PPIs reduce stomach acid and help manage symptoms, but they don’t reverse the cellular changes caused by long-term acid exposure. If you’ve had GERD for five or more years, you could still develop Barrett’s esophagus - the precancerous condition - even while on medication. That’s why endoscopic screening is still necessary for high-risk individuals.
Is Barrett’s esophagus the same as esophageal cancer?
No. Barrett’s esophagus is a precancerous condition where the lining of the esophagus changes due to chronic acid exposure. It’s not cancer yet, but it’s the only known pathway to esophageal adenocarcinoma. Most people with Barrett’s never develop cancer, but regular monitoring is critical because it allows doctors to catch abnormal cells early and remove them before they turn malignant.
How often should I get screened for Barrett’s esophagus?
If you’ve been diagnosed with Barrett’s esophagus without dysplasia (abnormal cells), guidelines recommend an endoscopy every 3 to 5 years. If low-grade dysplasia is found, you’ll need follow-up every 6 to 12 months. High-grade dysplasia often requires immediate treatment, like endoscopic removal of the abnormal tissue. Your doctor will tailor the schedule based on your individual risk and findings.
Can I lower my risk if I already have Barrett’s esophagus?
Absolutely. Quitting smoking, losing weight, taking PPIs consistently, and avoiding alcohol can reduce your risk of progression by up to 60%. Studies show that people who make these lifestyle changes and stick with regular endoscopic monitoring have dramatically lower chances of developing cancer. It’s not about being perfect - it’s about being consistent.
What if I’m not white or male - am I still at risk?
Yes. While white males over 50 have the highest risk, esophageal cancer can occur in anyone with long-term GERD. Women, younger people, and non-white individuals can develop Barrett’s esophagus and cancer too - just at lower rates. If you have chronic GERD (five+ years) and other risk factors like obesity, smoking, or a family history, you should still talk to your doctor about screening, regardless of your race or gender.




Ezequiel adrian
November 27, 2025 AT 11:14Bro, I’ve had heartburn since college and I still eat tacos at 2 a.m. 😅 Guess I’m just lucky? Or maybe my esophagus is made of titanium.
Deborah Williams
November 29, 2025 AT 02:02So let me get this straight - we’ve got a silent cancer train chugging along because we’d rather Google ‘is my burp normal?’ than let a camera into our throat? Classic American healthcare: treat the symptom, ignore the system, blame the patient when it’s too late. 🤷♀️
Brittany Medley
November 30, 2025 AT 08:38Just wanted to add: if you’re on PPIs long-term, get your B12 and magnesium checked. These meds can cause deficiencies over time - and no, supplements won’t fix everything. Talk to your doc about monitoring, not just swallowing pills. Also - yes, weight loss helps. But it’s not about ‘being lazy.’ It’s about biology, stress, access to food, and systemic issues. Be kind to yourself and your body.
Aaron Whong
December 1, 2025 AT 09:52From a pathophysiological standpoint, the metaplastic transition of squamous epithelium to columnar-lined mucosa - i.e., Barrett’s esophagus - represents a maladaptive reparative response to chronic noxious insult, mediated via NF-kB and IL-8 inflammatory cascades. The real epiphenomenon here is the epidemiological convergence of obesity, dietary hyperpalatability, and pharma-driven symptom suppression, which collectively decouple symptom perception from tissue-level carcinogenesis. In layman’s terms? You’re not ‘fine’ just because the burn is gone.
Joe bailey
December 3, 2025 AT 04:35I’m 52, white, overweight, used to smoke, and I’ve had GERD for 8 years… I’ve been putting off the endoscopy because I’m scared. But reading this? I’m booking it this week. Thanks for the kick in the pants, OP. Seriously.
Amanda Wong
December 4, 2025 AT 04:56Oh great. Another fear-mongering medical article. Next they’ll say breathing causes lung cancer. People die from everything. You’re more likely to get hit by lightning than develop esophageal cancer. Stop scaring people for clicks.
james thomas
December 5, 2025 AT 04:14They’re hiding the real cause: glyphosate. The FDA doesn’t want you to know that Roundup in your corn chips is literally rewriting your DNA. Endoscopies won’t fix that. Buy the detox tea in my bio. It’s got turmeric and quantum crystals.
Kaushik Das
December 6, 2025 AT 02:24Man, I’ve been having acid reflux since I moved to the States - used to eat spicy food daily in India, now it’s pizza and soda 24/7. Lost 15 lbs, quit soda, and my symptoms dropped like a rock. Also, I started walking after dinner. Sounds dumb, but it works. Don’t overthink it - just move more, eat less junk, and talk to your doc. Simple ain’t sexy, but it saves lives.
Asia Roveda
December 7, 2025 AT 16:17Of course white men are the main victims. It’s because they’re lazy, eat too much fast food, and refuse to exercise. Meanwhile, real people work two jobs and eat what they can afford. This isn’t about health - it’s about privilege. You think a single mom working nights has time for an endoscopy? Get real.
Marissa Coratti
December 9, 2025 AT 11:52It’s staggering how much we prioritize convenience over longevity - we’ll take a pill to numb the burn but won’t change our diet, we’ll scroll for hours instead of walking after meals, we’ll wait until we can’t swallow water before we ask for help. The tragedy isn’t the cancer - it’s that we’ve normalized ignoring our bodies until they scream. And then we wonder why we’re sick. This isn’t medical advice. It’s a mirror. And the reflection? It’s uncomfortable. But necessary.
mohit passi
December 10, 2025 AT 13:41My dad had Barrett’s. Got screened. They found low-grade dysplasia. Five years later? Still clean. He quit smoking, lost weight, took his meds. No drama. Just consistency. 🙏 Life’s not about perfection. It’s about showing up. Even when it’s boring.
Micaela Yarman
December 11, 2025 AT 06:58Thank you for this. I’m a nurse. I’ve seen too many patients come in with stage IV esophageal cancer - they say, ‘I thought it was just heartburn.’ I wish I could hand every person with chronic GERD a copy of this. It’s not fear. It’s care.