
Every year, tens of thousands of seniors end up in the hospital-not because of a fall, infection, or heart problem-but because of a medication they were told was safe. It’s not a rare mistake. It’s common. And it’s preventable.
If you or someone you love is over 65 and taking five or more pills a day, you’re not alone. About 40% of older adults in the U.S. are on five or more medications. That’s called polypharmacy. And while some of those drugs are essential, others are quietly putting lives at risk. The good news? You don’t have to guess which ones. There’s a clear, science-backed list called the Beers Criteria, updated in 2023, that tells doctors and families exactly which medications to question.
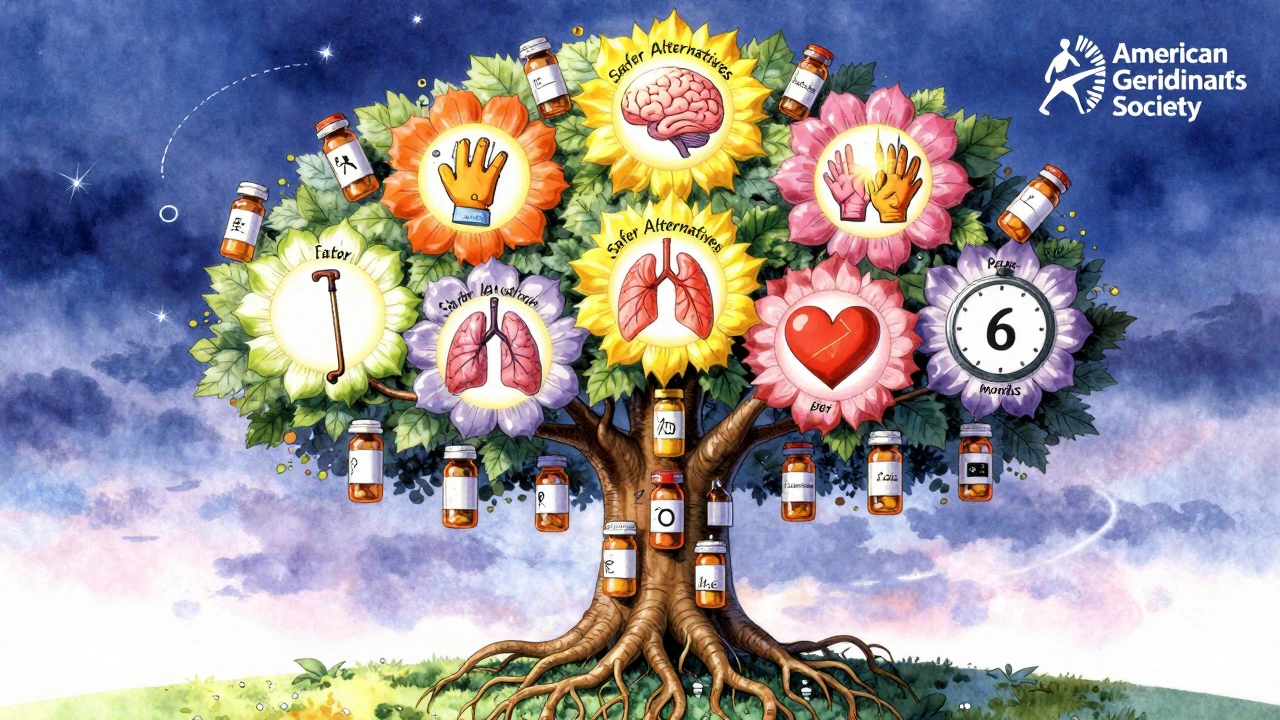
What the Beers Criteria Really Means for Seniors
The Beers Criteria isn’t just a list. It’s a warning system. Developed by the American Geriatrics Society and updated every two years, it identifies drugs that are more likely to cause harm than benefit in people over 65. These aren’t banned drugs. They’re drugs that, for younger people, might be fine-but for seniors, they carry hidden dangers.
Why? Because aging changes how your body handles medicine. Your kidneys slow down. Your liver doesn’t process drugs as fast. Your brain becomes more sensitive to sedatives. And when multiple drugs mix, the risks multiply. One study found that seniors on five or more medications are 2.5 times more likely to have a dangerous drug reaction than those on just two.
The 2023 update added five new high-risk medications and removed three others based on fresh evidence. That’s why reviewing your meds every six months isn’t optional-it’s lifesaving.
Top 5 High-Risk Medications Seniors Should Review
Not all risky drugs are obvious. Some are sold over the counter. Others are prescribed for decades without a second thought. Here are the five most dangerous ones-and what to ask your doctor instead.
1. Zolpidem (Ambien®) and Other Sleep Pills
Many seniors take zolpidem to help them sleep. But this drug doesn’t just help you fall asleep-it leaves you groggy, confused, and unsteady the next day. Studies show seniors on zolpidem have an 82% higher chance of falling. One in five of those falls leads to a broken hip. And the sedation can last up to 11 hours after taking it.
Worse, some people sleepwalk, eat, or even drive while under its influence-without remembering it later.
What to ask your doctor: “Can we try trazodone or cognitive behavioral therapy for insomnia instead?” These alternatives have far lower fall risks and don’t cause memory problems.
2. Glyburide (Diabeta®) for Diabetes
Glyburide is an old-school diabetes pill. It’s cheap. It’s been around for decades. But it’s also one of the most dangerous for seniors.
It can cause severe low blood sugar-so bad that 29.3% of seniors on glyburide end up in the ER. That’s nearly triple the rate of newer drugs like glipizide. And once blood sugar drops too low, it can trigger a stroke, seizure, or even death.
The FDA now requires a boxed warning on glyburide labels for patients over 65. That’s the strongest warning they can give.
What to ask your doctor: “Is glipizide or metformin a better option for me?” Both are safer, more predictable, and don’t carry the same hypoglycemia risk.
3. Diphenhydramine (Benadryl®) and Other Anticholinergics
You’ve probably seen this in allergy meds, sleep aids, and stomach remedies. It’s in Tylenol PM, Advil PM, and many generic cold pills. But diphenhydramine has an Anticholinergic Cognitive Burden (ACB) score of 3-the highest possible.
That means it blocks a brain chemical called acetylcholine. Over time, this increases dementia risk by 54% in seniors who take it for more than three years. One study found that people who took it daily for over 1,000 days had a 2.3-fold higher chance of developing Alzheimer’s.
It also causes dry mouth, constipation, urinary retention, and confusion. All of which can look like dementia-until you stop the drug.
What to ask your doctor: “Is there an antihistamine without anticholinergic effects?” Try loratadine (Claritin®) or cetirizine (Zyrtec®) for allergies. For sleep, melatonin or a non-drug approach is safer.
4. Nitrofurantoin (Macrobid®) for UTIs
This antibiotic is commonly prescribed for urinary tract infections in older women. But if your kidneys aren’t working well-common after 65-it can cause deadly lung damage.
Studies show seniors with even mild kidney decline (eGFR under 60) have a 12.8-fold higher risk of pulmonary toxicity from nitrofurantoin. In severe cases, it causes scarring in the lungs that can lead to permanent breathing problems or death.
Many doctors don’t check kidney function before prescribing it. That’s a dangerous gap.
What to ask your doctor: “Can we test my kidney function first? Is cephalexin or fosfomycin a safer option?” Both are just as effective and don’t carry the same lung risk.
5. Alpha-1 Blockers (Doxazosin, Prazosin, Terazosin)
These are often prescribed for high blood pressure or enlarged prostate. But they’re notorious for causing sudden drops in blood pressure when standing up. That’s called orthostatic hypotension.
Among seniors over 75, 24.7% of people on these drugs experience dizziness or fainting-more than double the rate of safer alternatives like chlorthalidone. One in three of those episodes leads to a fall.
They’re still used because they’re cheap. But the risk isn’t worth it.
What to ask your doctor: “Could we try an ACE inhibitor, ARB, or calcium channel blocker instead?” These control blood pressure without the dangerous dizziness.
How to Do a Medication Review at Home
You don’t need a PhD to protect yourself or a loved one. Here’s how to start a medication review today.
- Collect every pill, capsule, and patch. Put them all on the table-even vitamins, supplements, and over-the-counter meds. Don’t forget the cream for your arthritis or the eye drops for glaucoma.
- Write down what each one is for. If you don’t know why you’re taking it, that’s a red flag. Ask your pharmacist or doctor to explain each one.
- Check the Beers Criteria list. Go to the American Geriatrics Society website and search for “Beers Criteria 2023.” Compare your meds. If something matches, make a note.
- Ask these three questions at your next appointment:
- “Is this drug still necessary?”
- “Is there a safer alternative?”
- “Can we reduce the dose or stop one?”
- Bring someone with you. A spouse, child, or friend can help you remember what was said. Seniors often forget details during appointments.
Many doctors now use electronic alerts that flag Beers Criteria drugs. But if your doctor doesn’t mention them, don’t wait. Ask.

What Happens When You Switch to Safer Drugs?
It’s not just about avoiding harm. It’s about gaining life back.
One case study from Buckeye Health Plan followed a 79-year-old man who took glyburide, diphenhydramine, and zolpidem for years. He was always tired, confused, and had fallen twice. After switching to glipizide, loratadine, and melatonin, his energy improved. His memory cleared. He stopped falling. He started gardening again.
Another woman, 82, took nitrofurantoin for recurring UTIs. She developed shortness of breath and was diagnosed with lung scarring. Once she switched to fosfomycin, her breathing improved in weeks.
These aren’t rare miracles. They’re common outcomes when risky drugs are replaced.
Who Should Be Involved in the Review?
You don’t have to do this alone.
- Your primary care doctor leads the review and coordinates changes.
- A clinical pharmacist specializes in drug interactions and side effects. Many Medicare plans offer free medication reviews with a pharmacist.
- A geriatrician (a doctor who specializes in aging) can help if you’re on more than seven medications or have multiple chronic conditions.
- Your family can help track symptoms, notice confusion or dizziness, and remind you to ask questions.
Medicare now requires annual medication reviews for all beneficiaries. But you have to ask for it. Call your plan and say: “I want a Medication Therapy Management (MTM) session.”
What’s Changing in 2025?
The system is waking up. In January 2024, Medicare Advantage plans started tying 5% of their quality bonuses to how well they reduce high-risk medication use. That means insurers are now financially motivated to help you switch to safer drugs.
Pharmacies like CVS and Walgreens now use real-time alerts in their systems. When a doctor tries to prescribe zolpidem to a 78-year-old, the pharmacist’s screen flashes: “Beers Criteria Alert-High fall risk.”
Electronic health records from Epic and Cerner now auto-flag Beers Criteria drugs. If your doctor tries to write a prescription for glyburide for a senior, the system pops up: “Alternative recommended: glipizide.”
These aren’t just tech upgrades. They’re safety nets.
Final Thought: Your Meds Aren’t Set in Stone
Medications aren’t forever. Just because you’ve been taking something for five years doesn’t mean you still need it. Your body changes. Your health changes. Your risks change.
Every pill you take has a reason. But not every reason is still valid. The goal isn’t to stop all meds-it’s to stop the ones that are doing more harm than good.
Start today. Gather your pills. Write down the names. Ask one question at your next appointment. That’s all it takes to start protecting yourself-or someone you love-from a preventable hospital stay.
What are the most dangerous medications for seniors?
The most dangerous medications for seniors include zolpidem (sleep aids), glyburide (diabetes), diphenhydramine (allergy/sleep meds), nitrofurantoin (UTI antibiotic), and alpha-1 blockers like doxazosin (blood pressure/prostate). These are flagged in the 2023 Beers Criteria for causing falls, confusion, low blood sugar, lung damage, or sudden dizziness. Many are still prescribed because they’re cheap or familiar-but safer alternatives exist.
How do I know if my meds are high-risk?
Check the American Geriatrics Society’s Beers Criteria 2023 list. You can find it online for free. Look up each medication by name. If it’s listed, it’s flagged as potentially inappropriate for seniors. Also, ask your pharmacist: “Is this on the Beers list?” Most pharmacists know it by heart. If you’re on five or more drugs, a brown bag review with your doctor is essential.
Can I stop these medications on my own?
No. Never stop a medication suddenly-especially sleep aids, antidepressants, or blood pressure drugs. Stopping abruptly can cause seizures, rebound insomnia, or dangerous spikes in blood pressure. Always work with your doctor to taper off safely. For benzodiazepines or zolpidem, a 4- to 6-week gradual reduction is typical. For diabetes drugs like glyburide, switching to glipizide is usually done under close blood sugar monitoring.
Are over-the-counter meds safe for seniors?
Not always. Many OTC sleep aids and allergy meds contain diphenhydramine or doxylamine-both high-risk anticholinergics. Tylenol PM, Advil PM, Benadryl, and store-brand sleep aids often contain these. Even cold medicines can have hidden anticholinergics. Always read the “Active Ingredients” label. If you see diphenhydramine, doxylamine, or chlorpheniramine, assume it’s risky. Use loratadine, cetirizine, or melatonin instead.
How often should seniors review their medications?
At least once a year, but every six months is better if you’re on five or more medications. Change your meds? Review again. Had a fall? Review. Got a new diagnosis? Review. Many Medicare Advantage plans offer free medication reviews with a pharmacist. Call your plan and ask for a Medication Therapy Management (MTM) session-it’s covered.



Andrea Beilstein
December 7, 2025 AT 20:17It's wild how we treat aging like a glitch to be fixed with pills instead of a natural process that needs rethinking
I've seen grandmas on 12 meds who could barely walk, then after a review, down to three and suddenly gardening again
It's not about longevity-it's about living, not just existing
Why do we accept confusion and falls as 'just part of getting old' when the fix is often just stopping something?
Lisa Whitesel
December 9, 2025 AT 06:22Of course doctors keep prescribing these. They're paid by volume, not outcomes. The system is broken
And don't get me started on pharma ads targeting seniors-'Sleep better tonight!' while hiding the fact it could kill you
It's not negligence-it's profit-driven malpractice
Katie Harrison
December 9, 2025 AT 08:52Thank you for sharing this-so many families don’t know where to start.
I helped my mother review her meds last year; she was on diphenhydramine nightly for ‘sleep,’ and it was making her hallucinate at 3 a.m.
Switched to melatonin and a sound machine. She’s been sleeping like a teenager again.
But the hardest part? Getting the doctor to listen. He said, ‘It’s been working for ten years.’
So we got a second opinion. And a pharmacist. And a spreadsheet.
It’s exhausting. But worth it.
Every senior deserves to wake up clear-headed-not foggy from a drug that was never meant for them.
Christian Landry
December 9, 2025 AT 13:59bro i had no idea benadryl was this bad 😳
i give it to my pops every time he gets a cold
just switched him to claritin last week-no more ‘forgetting where he put his keys’ after dinner
thanks for the heads up!! 🙏
Sabrina Thurn
December 10, 2025 AT 04:10From a clinical pharmacy standpoint, the Beers Criteria is one of the most underutilized tools in geriatric care
The real issue isn’t the drugs-it’s the lack of deprescribing protocols in primary care
Most clinicians aren’t trained in polypharmacy risk stratification, and time constraints prevent comprehensive reviews
MTM sessions under Medicare are a step forward, but uptake is low because patients don’t know to ask for them
Pharmacists are the unsung heroes here-they’re the ones catching these errors at the counter, often without reimbursement
Systemic change requires both education and financial incentives
And yes, the EHR alerts are helping-but they’re only as good as the clinician who sees them
Mona Schmidt
December 10, 2025 AT 11:25There’s a quiet epidemic here, and it’s not just about medications-it’s about how we treat aging as a medical problem rather than a human experience
We’ve turned elders into collections of symptoms to be managed, not people to be heard
I’ve sat with my 84-year-old neighbor while she read her pill bottle labels aloud, confused, because no one ever explained why she was taking five things
Her doctor assumed she understood. She didn’t want to admit it
That’s the real danger: silence
It’s not just glyburide or zolpidem-it’s the refusal to sit down, listen, and ask: ‘What do you want your life to look like?’
When we stop seeing seniors as patients and start seeing them as people with stories, we stop prescribing fear and start prescribing dignity
And yes, I’ve printed the Beers Criteria and taped it to my fridge
Because someone has to remember for them
Guylaine Lapointe
December 11, 2025 AT 10:42Ugh, another feel-good article pretending this is a personal responsibility issue
It’s not about asking your doctor-most seniors can’t even afford to go
It’s about insurance companies refusing to cover safer alternatives because they’re more expensive
And don’t get me started on how Medicaid still pays for glyburide like it’s 1995
Stop blaming families for not doing enough
The system is rigged
And you’re all just rearranging deck chairs
Larry Lieberman
December 12, 2025 AT 00:02Just had my aunt’s med review today 😮
She was on nitrofurantoin for 8 years… kidney function was at 48
Switched to fosfomycin-no more shortness of breath
She’s back to knitting and even went to the park today 🌞
Why isn’t this standard???