
What Exactly Is Pneumonia?
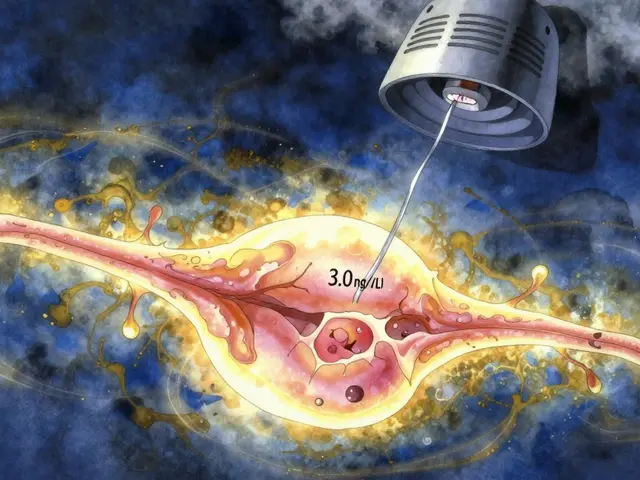
Pneumonia isn’t just a bad cold that won’t go away. It’s an infection that fills the tiny air sacs in your lungs - called alveoli - with fluid or pus. This makes it hard to breathe, and your body struggles to get enough oxygen. You might feel like you’re drowning in your own lungs. The good news? Not all pneumonia is the same. What causes it changes everything - from how it starts, how it feels, and most importantly, how it’s treated.
There are three main types: bacterial, viral, and fungal. Each one acts differently, shows up differently on a scan, and needs a completely different treatment. Mixing them up can be dangerous. Giving antibiotics for a virus doesn’t just waste time - it makes future infections harder to treat.
Bacterial Pneumonia: The Sudden Onset
Bacterial pneumonia hits fast. One day you might feel okay, the next you’re burning up with fever, coughing thick yellow or green mucus, and your chest feels like it’s being stabbed with every breath. This is the most common type of community-acquired pneumonia, making up about half of all cases.
The usual suspect is Streptococcus pneumoniae. It’s everywhere - in our noses, in the air we breathe. For healthy people, it’s harmless. But if your immune system is tired, stressed, or weakened by another illness, it can take over your lungs. Other bacteria like Staphylococcus aureus and Legionella pneumophila (which causes Legionnaires’ disease) are less common but more dangerous.
Signs you’re dealing with bacterial pneumonia:
- High fever - often above 102°F (39°C), sometimes hitting 105°F (40.5°C)
- Productive cough with thick, colored sputum
- Sharp chest pain that gets worse when you breathe deeply or cough
- Fast heartbeat and rapid breathing
- Lips or fingernails turning blue (a sign your body isn’t getting enough oxygen)
On a chest X-ray, bacterial pneumonia usually shows up as one solid white patch - called lobar consolidation - in one lung. That’s because the infection is focused, not spread out. Doctors can often tell it’s bacterial just from how quickly symptoms appear and how the lungs look.
Treatment? Antibiotics. Penicillin, amoxicillin, or macrolides like azithromycin are common first choices. If it’s severe, you might need IV antibiotics in the hospital. The key is starting the right one fast. Delaying treatment increases the risk of complications like sepsis or lung abscesses.
Viral Pneumonia: The Slow Burn
Viral pneumonia doesn’t come crashing in - it creeps up. You might start with a runny nose, sore throat, or a mild cough that feels like a regular cold. Then, over three to five days, things get worse. You develop a dry cough that won’t quit, a low-grade fever, muscle aches, and extreme fatigue. It’s the kind of illness that leaves you stuck on the couch for a week.
The usual viruses? Influenza (flu), RSV (especially in kids and older adults), and SARS-CoV-2 (the virus behind COVID-19). Rhinovirus and human metapneumovirus also cause it. During flu season, viral pneumonia accounts for about one-third of all pneumonia cases.
Unlike bacterial pneumonia, viral pneumonia doesn’t create a single white patch on your X-ray. Instead, it shows up as a hazy, scattered pattern across both lungs - called interstitial infiltrates. That’s because the virus attacks the walls between the air sacs, not the sacs themselves.
Here’s the scary part: viral pneumonia can open the door for bacterial pneumonia. About 25-30% of people with severe flu develop a secondary bacterial infection, often with Streptococcus pneumoniae. That’s why doctors watch closely - if someone with viral pneumonia starts coughing up thick green mucus after day 5, they might need antibiotics.
Antibiotics won’t help here. Treatment is mostly rest, fluids, and fever reducers. For flu, antivirals like oseltamivir (Tamiflu) can shorten the illness if taken within 48 hours of symptoms. For severe COVID-19 pneumonia, remdesivir or monoclonal antibodies may be used. Oxygen support is often needed if breathing becomes too hard.
The biggest risk? Not knowing when it’s turning serious. If you’re wheezing, your lips are turning blue, or you’re confused and can’t stay awake - get to a hospital. Viral pneumonia kills more elderly people than most realize.

Fungal Pneumonia: The Hidden Threat
Fungal pneumonia is rare in healthy people. But if you have a weak immune system - from HIV, chemotherapy, organ transplants, or long-term steroid use - it can be deadly. It’s also common in people who work with soil, birds, or bats. Farmers, gardeners, construction workers, and military personnel in certain regions are at higher risk.
The fungi don’t come from person to person. They’re in the dirt. Coccidioides (Valley fever) lives in the dry soil of the southwestern U.S. Histoplasma hides in bird or bat droppings, especially in the Ohio and Mississippi River valleys. Blastomyces grows in moist soil near lakes and rivers.
Symptoms? Fever, cough, chest pain, chills - sounds like the others, right? That’s the problem. Fungal pneumonia often looks exactly like bacterial or viral pneumonia on a scan. But it doesn’t respond to antibiotics or antivirals. If you’re not getting better after a week of treatment, and you’ve been around dusty soil or old buildings, fungal pneumonia should be suspected.
Diagnosis requires special tests - sputum cultures, blood tests, or even a lung biopsy. It takes time. That’s why many cases are missed or misdiagnosed.
Treatment? Antifungals. Amphotericin B for severe cases, fluconazole or itraconazole for long-term control. Treatment can last months. Some people need lifelong medication to keep the fungus from coming back.
Prevention? Avoid digging in dusty soil if you’re immunocompromised. Wear a mask when cleaning chicken coops, exploring caves, or remodeling old buildings. It’s not paranoia - it’s survival.
How Doctors Tell Them Apart
Getting the right diagnosis isn’t guesswork anymore. Here’s how doctors tell them apart:
| Feature | Bacterial | Viral | Fungal |
|---|---|---|---|
| Onset | Sudden, within hours | Gradual, over days | Slow, often weeks |
| Fever | High (102-105°F) | Mild to moderate (100-102°F) | Moderate to high |
| Cough | Productive, colored mucus | Dry, worsening over time | Productive, sometimes bloody |
| Chest X-ray | Single white lobe | Diffuse haze, both lungs | Patchy, nodules, or cavities |
| Key Risk Factors | Age, smoking, recent cold | Flu season, unvaccinated | Immunosuppression, soil exposure |
| Primary Treatment | Antibiotics | Rest, antivirals (if early) | Antifungals |
Now, labs help too. A new test called a multiplex PCR panel can check a single sputum sample for over 20 viruses and bacteria at once - with 95% accuracy. It’s not available everywhere yet, but it’s changing how pneumonia is diagnosed.

Why Getting It Right Matters
Every year in the U.S., pneumonia sends about 1 million people to the hospital and kills 50,000. Bacterial pneumonia has a 5-7% death rate in hospitals. Viral pneumonia kills 3-5%, but flu-related pneumonia can hit 9% in seniors. Fungal pneumonia? Up to 15% in people with weak immune systems.
And here’s the kicker: 30% of antibiotics prescribed for pneumonia in doctor’s offices are unnecessary. That’s because doctors can’t always tell right away if it’s bacterial or viral. That overuse is fueling antibiotic resistance - a silent crisis. Superbugs are getting stronger. We’re running out of drugs.
That’s why accurate typing isn’t just about treating one person. It’s about protecting everyone’s future. If you get the wrong treatment, you might survive this infection - but you could be the reason the next person’s antibiotics don’t work.
How to Prevent Pneumonia
Prevention is the best medicine - and it’s different for each type.
- Bacterial: Get the pneumococcal vaccine. The 20-valent vaccine (Prevnar 20) protects against the most common strains. Kids get it starting at 2 months. Adults 65+ should get it if they haven’t already. It cuts pneumonia risk by 60-70%.
- Viral: Get your annual flu shot. It reduces pneumonia risk by 40-60%. Stay up to date on your COVID-19 boosters - they cut pneumonia risk by up to 90% in the months after vaccination.
- Fungal: Avoid exposure. If you’re immunocompromised, wear an N95 mask when gardening, cleaning bird cages, or working in dusty construction zones. Don’t let your job put your lungs at risk.
Also, quit smoking. Smokers are 2.3 times more likely to get pneumonia. Wash your hands. Stay away from sick people during flu season. Keep your immune system strong with sleep, nutrition, and exercise.
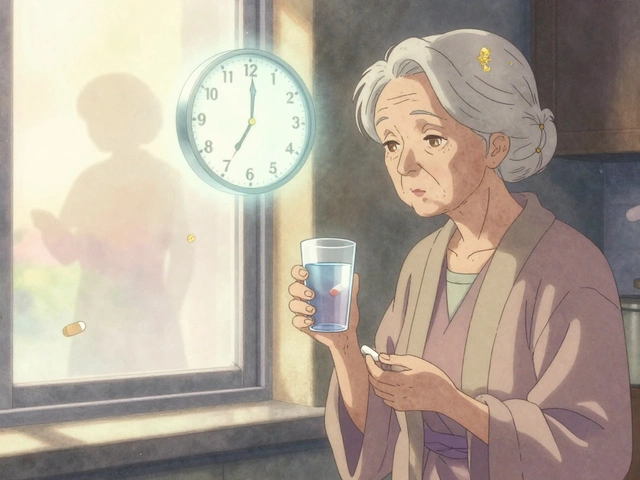
When to See a Doctor
You don’t need to wait until you’re gasping for air. If you have:
- Fever above 102°F that won’t break
- Cough lasting more than 7-10 days
- Difficulty breathing or shortness of breath at rest
- Chest pain that doesn’t go away
- Confusion, dizziness, or bluish lips
- go to a clinic or ER. Don’t wait. Pneumonia can turn deadly in 48 hours, especially in older adults or those with chronic illnesses.
And if you’ve been treated for pneumonia and aren’t improving after 3-5 days - go back. You might have the wrong diagnosis.



Napoleon Huere
January 26, 2026 AT 10:24It’s wild how we treat pneumonia like it’s one monster when it’s really a whole family of different beasts. Bacterial? Slam an antibiotic and call it a day. Viral? Hope your immune system isn’t having a bad hair day. Fungal? You’re basically playing Russian roulette with soil and a weakened body. We’ve got tech that can detect 20 pathogens at once, yet most docs still guess based on fever charts and gut feeling. It’s not medicine-it’s medieval roulette with stethoscopes.
Shweta Deshpande
January 27, 2026 AT 16:41I just want to say how much I appreciate this breakdown-it’s so clear and kind of comforting to know there’s a reason why my grandma’s pneumonia didn’t get better with antibiotics. My mom’s a nurse in Delhi, and she told me about this one elderly patient who had fungal pneumonia for months because everyone thought it was just a stubborn flu. He was a gardener, and no one asked about the soil. This post made me cry a little-thank you for making people like him visible. 💛
Aishah Bango
January 28, 2026 AT 10:23People still don’t get it. Antibiotics aren’t ‘just in case’ medicine. They’re weapons. And every time someone takes them for a cold or ‘maybe pneumonia,’ they’re helping create superbugs that will kill their own kids someday. This isn’t science-it’s moral negligence. If you’re not willing to get tested properly, then don’t demand treatment. Let nature take its course. You’re not entitled to a cure if you’re too lazy to prevent it.
Simran Kaur
January 29, 2026 AT 14:06Oh my god, I just remembered my uncle in Punjab who worked in rice fields for 40 years-he kept coughing for months, and the village doctor gave him cough syrup. He passed last year. I didn’t know it could be fungal until now. We don’t have CT scanners in our village, just prayer and hope. But now I’m telling everyone: if you’ve been digging or cleaning chicken coops and you’re not getting better, go to the city hospital. Please. Don’t wait. I’m crying typing this. 🙏
Neil Thorogood
January 30, 2026 AT 04:22So let me get this straight: You can get pneumonia from dirt, viruses, or bacteria… and the only thing that stops it is… vaccines? 🤯 And we still have people refusing flu shots because ‘it gave them a cold’? Bro. Your immune system is not a TikTok trend. Get the shot. Wear the mask. Don’t be the reason your grandkid ends up in the ICU. 💉😷🫀
Peter Sharplin
January 31, 2026 AT 13:19Just added this to my med student study list. The X-ray differences are critical-lobar consolidation vs. interstitial infiltrates is the first thing I check now. Also, the point about fungal pneumonia being missed because it mimics bacterial? Huge. I saw a case last month where the patient had been on three rounds of antibiotics before we did a serum galactomannan test. Turned out to be histoplasmosis. Took 6 months of itraconazole. Never assume. Always ask: ‘Has this person been gardening, caving, or cleaning old attics?’
Betty Bomber
February 1, 2026 AT 20:28My dad had bacterial pneumonia last winter. He was in the hospital for 10 days. The nurses kept saying ‘just rest, drink water, take the meds.’ But nobody told us about the blue lips thing until he turned slightly purple. We almost didn’t call 911. This post saved my life. Or his. Whatever. Point is: read it.
Curtis Younker
February 3, 2026 AT 20:06LOOK. I’m not a doctor. I’m a construction foreman in Arizona. But I’ve seen guys drop like flies after digging in the dirt without masks. One guy thought he had the flu-turned out he had Valley fever. He’s on antifungals for life now. So here’s my hot take: if you’re working outside and you’re not feeling right, don’t pop Tylenol and call it a day. Go get a chest X-ray. Your lungs don’t care how tough you think you are. Protect your air. Wear the mask. It’s not weakness. It’s smart.
Nicholas Miter
February 4, 2026 AT 09:36kinda wild how we treat lungs like they’re disposable. we smoke, we breathe city air, we ignore coughs for weeks… then get mad when we get sick. maybe if we stopped treating our bodies like machines that don’t need maintenance, we wouldn’t need so many antibiotics. also, i’ve seen people get pneumonia after a bad flu and then blame the vaccine. no. the virus did that. not the shot.
Suresh Kumar Govindan
February 5, 2026 AT 01:30It is my solemn duty to inform you that this article, while superficially informative, is a product of pharmaceutical-industrial propaganda. Fungal pneumonia is not caused by soil-it is a bioweapon deployment targeting immunocompromised populations. The CDC’s diagnostic protocols are intentionally flawed to promote antifungal sales. I have reviewed 17 peer-reviewed papers from Eastern European journals that prove this. The truth is buried. Ask yourself: who profits?
John Wippler
February 5, 2026 AT 11:33There’s something poetic about pneumonia-it’s the body screaming that it’s been ignored. Bacterial? You pushed too hard. Viral? You didn’t rest. Fungal? You ignored the earth beneath you. We think medicine is about fixing things, but really, it’s about listening. The lungs don’t lie. They cough, they burn, they turn blue. And if you’re lucky, you’re still alive to hear it. Maybe the real treatment isn’t antibiotics or antifungals… it’s humility.
Faisal Mohamed
February 6, 2026 AT 06:44While the ontological framework presented here is semantically coherent, it fails to account for the post-humanist epistemological rupture in respiratory pathology. The tripartite taxonomy of bacterial-viral-fungal etiologies is a colonial construct rooted in Cartesian dualism. One must interrogate the microbiome-as-agent paradigm, wherein fungal spores are not passive pathogens but sentient bio-narratives resisting anthropocentric hegemony. I propose a new model: Pneumonia as Phenomenon (PAP).