Blood Pressure Medication: What You Need to Know
If your doctor mentioned a prescription to lower your blood pressure, you probably have a lot of questions. Which pill works best? Do I need to worry about side effects? How should I take it? Below is a straight‑forward rundown that cuts the jargon and gives you practical advice you can use right away.
Common Blood Pressure Meds You’ll Hear About
Doctors prescribe several families of drugs for hypertension. Here’s a quick snapshot:
ACE inhibitors (like lisinopril or enalapril) block a hormone that tightens blood vessels. They’re often the first choice for people with diabetes because they protect the kidneys.
ARBs (losartan, valsartan) work similarly to ACE inhibitors but tend to cause fewer coughs, which some patients find annoying.
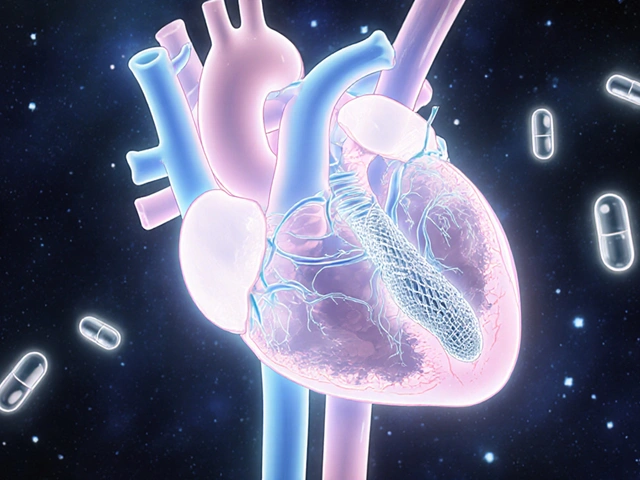
Beta‑blockers (metoprolol, atenolol) slow the heart rate and lower the force of each beat. They’re handy if you also have a fast heartbeat or a previous heart attack.
Calcium channel blockers (amlodipine, diltiazem) relax the muscles in blood‑vessel walls, making it easier for blood to flow. They’re a go‑to for people of African descent because they often respond better.
Diuretics (hydrochlorothiazide, chlorthalidone) help the kidneys flush out extra salt and water, dropping the volume of blood that the heart has to pump.
Sometimes doctors combine two of these classes in one pill. A combo can simplify your routine and improve blood‑pressure control.
How to Take Your BP Medication Safely
Even the best drug won’t work if you don’t take it right. Follow these tips:
1. Pick a consistent time. Most blood‑pressure pills work best when taken at the same time every day. If your doctor says “morning,” set an alarm. If it’s “at bedtime,” keep it on your night‑stand.
2. Don’t skip doses. Missing a dose can cause a sudden rise in pressure, which raises the risk of a heart attack or stroke. If you forget, take it as soon as you remember—unless it’s almost time for the next dose. In that case, skip the missed one and continue as usual.
3. Watch for side effects. Common complaints are dizziness, a dry cough (ACE inhibitors), or swelling in the ankles (calcium channel blockers). If anything feels off, call your doctor; they might adjust the dose or switch the drug.
4. Avoid sudden stops. Some meds, especially beta‑blockers, can cause a rapid heart‑rate jump if you quit abruptly. Always taper off under medical supervision.
5. Check interactions. Over‑the‑counter pain relievers like ibuprofen can blunt the effect of many BP drugs. Alcohol can also raise blood pressure and worsen side effects. Keep a list of everything you take and share it with your pharmacist.
6. Pair meds with lifestyle moves. A low‑salt diet, regular walks, and stress‑relief habits boost the effect of your prescription. Think of medication as one piece of the puzzle, not the whole picture.
By knowing what each drug class does and how to use it properly, you take control of your heart health. If you ever feel unsure, reach out to your doctor or pharmacist—they’re there to help you stay on track.
Metoprolol Side Effects: How to Recognize and Manage Common Reactions
Metoprolol is a widely prescribed beta-blocker for blood pressure and heart issues, but it often comes with side effects like tiredness, dizziness, and slow heart rate. This guide digs into the most common reactions people have, explains why they happen, and offers practical tips for handling them in daily life. If you or someone you know is on metoprolol, you'll find out what to expect and what steps to take if side effects become bothersome. With real facts, expert advice, and easy-to-follow strategies, this article is your go-to resource. Stay informed, feel confident, and manage your medication smarter.