
For many people with gout, the pain comes and goes like a storm-sudden, fierce, and exhausting. But what if the real problem isn’t just the flare-ups, but what’s happening quietly in your blood the whole time? That’s where urate targets come in. This isn’t about waiting for pain to return. It’s about keeping your serum urate levels low enough to stop crystals from forming, dissolve existing ones, and truly take control of the disease.
What Exactly Is a Urate Target?
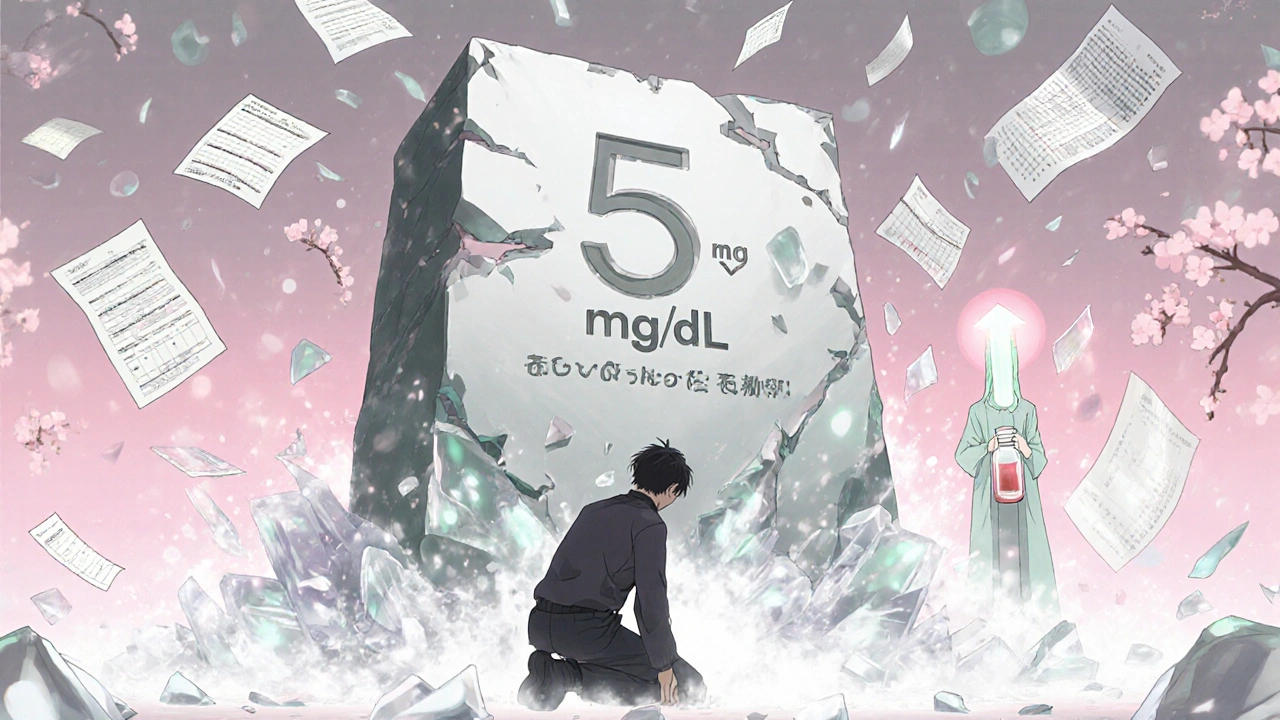
Serum urate is the amount of uric acid floating in your blood. When it hits 6.8 mg/dL or higher, it starts to form sharp, needle-like crystals in your joints. That’s what triggers a gout attack. But here’s the key: you don’t need to wait for a flare to start treatment. The goal is to keep your levels below the saturation point. Major guidelines from the American College of Rheumatology (ACR), NICE, and EULAR all agree on the same baseline target: below 6 mg/dL (or 360 micromol/L). This isn’t arbitrary. Studies show that when you hold urate below this level, flare frequency drops by 74%. For people with tophi (those visible lumps under the skin), chronic joint damage, or frequent flares despite treatment, the target gets even stricter: below 5 mg/dL (300 micromol/L). That’s the difference between managing symptoms and actually reversing damage.Why Allopurinol Is Still the First Choice
Allopurinol has been around since the 1960s, but it’s not outdated-it’s proven. It works by blocking xanthine oxidase, the enzyme that makes uric acid. Most guidelines, including the 2020 ACR and EULAR 2023, recommend it as the first-line drug, especially if your kidneys are working normally. But here’s the catch: most people start too low and never increase the dose. Doctors often begin with 100 mg a day, sometimes even 50 mg if kidney function is reduced. That’s fine for mild cases, but for most people with gout, that’s not enough. Real-world data from New Zealand shows that 30-50% of patients need more than 300 mg daily to hit their target. Some even need 600-800 mg a day-and it’s safe if you’re monitored properly. The trick? Start low, go slow, and check your blood every 4-6 weeks. Increase the dose by 50-100 mg each time until you hit your target. Don’t stop because you had a flare. That’s normal in the first few months. The crystals are dissolving, and your body is reacting. Keep going.Febuxostat: When Allopurinol Doesn’t Cut It
Febuxostat is a newer option. It also blocks uric acid production, but it’s processed differently by the liver instead of the kidneys. That makes it a good alternative if you have moderate to severe kidney disease. A 2023 meta-analysis found it achieves target urate levels 15% more often than allopurinol in patients with CKD stage 3 or worse. It’s also useful if you’ve had an allergic reaction to allopurinol-even though true hypersensitivity (like allopurinol hypersensitivity syndrome) is rare (0.1-0.4%). Still, if you’re HLA-B*5801 positive, your risk jumps 25-fold. That’s why some places test for this gene before starting allopurinol, especially in populations like Māori and Pacific peoples, where the gene variant is more common. Febuxostat starts at 40 mg a day. If your urate doesn’t drop below 6 mg/dL after a month, bump it to 80 mg. That’s it. No need to go higher. It’s not stronger than allopurinol at maximum doses-it just works better for some bodies.
What About the 5 mg/dL Target? Is It Real?
You’ll hear doctors say, “Aim for 5 mg/dL if you have tophi.” But here’s the truth: no large randomized trial has proven that 5 mg/dL is better than 6 mg/dL for dissolving tophi. The evidence comes from observational studies showing that people who hit <0.30 mmol/L lost more tophi over time. One study showed an 89% reduction in tophus burden at that level, compared to 72% at <0.36 mmol/L. That’s why EULAR calls it a “treat-to-dissolve” strategy. It’s not just about avoiding flares anymore. It’s about erasing the damage. If you have visible tophi, your doctor should consider imaging-like dual-energy CT-to confirm crystal presence. Only then should you push for the lower target. Don’t chase 5 mg/dL blindly. If you’re already at 5.5 mg/dL and haven’t had a flare in a year, you might not need to go lower.The Biggest Problem? Not Taking It Seriously
Here’s the hard truth: only 42% of gout patients reach their urate target within a year. Why? Three big reasons:- Doctors don’t titrate enough. Many start a patient on 100 mg of allopurinol and never touch it again. That’s like giving aspirin for a broken leg.
- Patients fear side effects. Most are scared of allopurinol because they’ve heard stories of rashes or reactions. But the risk is tiny if you start low and go slow. And if you do get a rash, stop it-but don’t assume you can’t try again.
- No monitoring. If you don’t test your serum urate, you’re flying blind. Studies show monthly testing during titration boosts success by 31%. Yet in the U.S., only 54% of patients get even quarterly tests.
What About Asymptomatic High Urate?
If your urate is 7 mg/dL but you’ve never had a flare? Don’t start medication. The ACR is clear: treat gout, not just high numbers. There’s no proof that lowering urate in people without symptoms prevents future flares or kidney damage. Lifestyle changes-cutting alcohol, reducing sugary drinks, losing weight-are the right first step. Medication is only for those who’ve already had attacks.What’s Next? The Future of Gout Treatment
New tools are coming. The GOUT-PRO study in 2024 showed that testing for genetic variants like ABCG2 and SLC22A12 can predict how well someone responds to allopurinol. People with certain gene patterns need higher doses. Genotype-guided dosing raised target achievement from 61% to 83% in just six months. Another drug, verinurad, is in late-stage trials. It works differently-it helps your kidneys flush out more uric acid. That could mean fewer dose escalations and better results for people who don’t respond to allopurinol or febuxostat. And the ULTRA-GOUT trial, expected to finish in late 2025, will compare fixed-dose allopurinol versus treat-to-target. If the latter wins, it could change how every doctor treats gout.What You Can Do Today
If you have gout and aren’t at your target:- Ask your doctor for a serum urate test-right now.
- If you’re on allopurinol and your dose is under 300 mg/day, ask if it’s time to increase.
- If you’re on febuxostat and still above 6 mg/dL, ask about going to 80 mg.
- Request monthly testing during the first 6 months.
- Don’t stop your meds because of a flare. That’s part of the process.
How long does it take to reach a urate target with allopurinol?
Most people need 6 to 12 months to reach their target, especially if they start at a low dose. It’s not a quick fix. Dose increases every 4-6 weeks, with blood tests in between, are key. Some patients need doses over 600 mg/day to get there, and that’s normal if tolerated.
Can I stop taking allopurinol if I haven’t had a flare in a year?
No. Stopping medication will let urate levels rise again, and crystals will reform. Gout is a chronic condition that requires ongoing management. Even if you’re flare-free, you still need to maintain your urate target to prevent long-term joint damage and tophi.
Is febuxostat safer than allopurinol?
It depends. Febuxostat doesn’t cause the rare but serious allopurinol hypersensitivity syndrome, so it’s safer for people with HLA-B*5801 or past reactions. But it carries a slightly higher risk of heart-related death in patients with existing cardiovascular disease. If you have heart issues, your doctor should weigh this carefully. For most others without heart disease, both are safe when used correctly.
Why do I get more flares when I start or increase my gout medication?
That’s called the "flare paradox." When urate-lowering drugs dissolve crystals, they release particles that trigger inflammation. It’s not the drug failing-it’s working. Most guidelines recommend starting a low-dose colchicine or NSAID at the same time as ULT to prevent these flares. Don’t stop your urate-lowering medicine because of this. Keep going, and the flares will settle.
Do I need to get my urate tested if I feel fine?
Yes. You can feel fine and still have urate levels above 6 mg/dL. Gout damage builds silently. Blood tests are the only way to know if your treatment is working. Even if you haven’t had a flare in years, you still need to monitor your urate to prevent joint erosion and tophi.
What if I can’t reach my target even on high doses of allopurinol?
That’s called refractory gout. About 46% of patients don’t reach target even on max doses. Options include switching to febuxostat, adding a uricosuric like probenecid (if kidneys are good), or newer drugs like pegloticase for severe cases. Talk to a rheumatologist. There are more tools than you think.




Matthew Mahar
November 22, 2025 AT 17:39Okay but like… I’ve been on allopurinol for 3 years and still get flares. I thought we were supposed to be below 6? My last bloodwork was 6.4. I feel like my doc just gives me the pill and says ‘come back in a year.’ No one checks in. No one cares. I’m tired of being the guy who ‘just needs to try harder.’
John Mackaill
November 23, 2025 AT 14:02There’s a quiet revolution happening in gout care-and it’s not about fancy new drugs. It’s about consistency. Most people don’t realize that allopurinol isn’t a pill you take when it hurts-it’s a daily commitment to your future joints. I’ve seen patients go from wheelchair-bound to hiking again just by hitting that 5 mg/dL target. It takes patience. And blood tests. And not giving up when the first flare hits.
Casper van Hoof
November 24, 2025 AT 00:51The empirical basis for the 5 mg/dL threshold remains largely inferential, derived from longitudinal observational cohorts rather than randomized controlled trials with hard endpoints such as tophi regression or joint preservation. While clinically pragmatic, the elevation of this target to a de facto standard may reflect therapeutic optimism over robust evidence.
Richard Wöhrl
November 24, 2025 AT 03:18Important note: If you’re on allopurinol and you get a flare in the first 3–6 months-DON’T STOP. Seriously. It’s not the drug failing. It’s your body flushing out crystals. That’s inflammation from dissolving crystals, not a new attack. Keep the dose going. Check your urate every 4–6 weeks. Increase by 50–100 mg until you hit target. And yes, 600–800 mg is safe if you’re monitored. I’ve had patients on 900 mg. No issues. Just regular labs.
Pramod Kumar
November 24, 2025 AT 12:28Bro, I used to think gout was just ‘drinking too much beer’-until my big toe turned purple and I couldn’t wear shoes for a month. Then I learned it’s not about booze, it’s about crystals. And those crystals? They’re like tiny glass shards in your joints, slowly eating away at your bones. Allopurinol isn’t magic-it’s a daily shield. Febuxostat? It’s like switching from a rusty sword to a laser blade if your kidneys are weak. But you gotta stick with it. No flares = no more crying in the bathroom at 3 a.m.
Brandy Walley
November 25, 2025 AT 01:52shreyas yashas
November 25, 2025 AT 03:25Man, I get it. I was on 100mg allopurinol for two years. My doc said ‘it’s working.’ But I was still flaring every 2 months. Finally switched to 400mg. Zero flares in 18 months. The dose matters. Not the brand. Not the hype. Just the number. And yeah, blood tests. Don’t skip them. They’re your only real cheat code.
Katy Bell
November 26, 2025 AT 20:50I just want to say thank you to whoever wrote this. I’ve been scared to talk about my gout because people think I’m just ‘a drunk guy.’ But this? This is real. I’m on 600mg allopurinol. My urate is 4.9. I can walk again. I’m not cured-but I’m not broken anymore. And that’s enough.
Ragini Sharma
November 27, 2025 AT 11:54so febuxostat is just allopurinol but for people who dont wanna risk their liver?? also why is everyone so obsessed with numbers? like its not like urate is a tiktok follower count 😭
Linda Rosie
November 27, 2025 AT 15:32Thank you for this clear, evidence-based overview. The distinction between 6 mg/dL and 5 mg/dL targets is clinically significant and often underemphasized in primary care. Consistent monitoring and dose titration remain underutilized but critical components of long-term gout management.