
Generic drugs make up 90% of all prescriptions filled in the U.S., yet they only cost 10% of what brand-name drugs do. That’s a win for patients and healthcare systems-but not always for the companies making them. In 2025, the U.S. generic drug market brought in $35 billion, down 6.1% over five years. Meanwhile, companies like Teva lost $174 million last year. How is that possible? How can something so essential to affordable healthcare be so unprofitable?
The Commodity Trap
The simplest generic drugs-like metformin for diabetes or lisinopril for high blood pressure-are made by dozens of manufacturers. When a patent expires, everyone rushes in. Prices drop fast. One company cuts its price by 5%, the next drops it by 10%. Soon, the drug sells for pennies per pill. Gross margins? Sometimes under 30%. A decade ago, they were 50-60%. This isn’t innovation. It’s a race to the bottom. The FDA approved over 1,000 generic drugs in 2022 alone. Each one adds to the pile. Manufacturers compete not on quality, but on who can make it cheapest. The problem? Making cheap drugs still costs a lot. Setting up a cGMP-compliant factory runs over $100 million. Each ANDA application to the FDA averages $2.6 million. And once you’re in, you’re stuck in a price war with no way out. Many small players can’t survive. A 2024 McKinsey study found that over 65% of new entrants focusing only on commodity generics fail within two years. They can’t afford the upfront costs, the regulatory delays, or the price collapses. The result? Fewer suppliers. Fewer choices. And sometimes, no one makes the drug at all.The Shift to Complex Generics
Not all generics are created equal. Some drugs are hard to copy. Think inhalers with precise dosing, injectables that need sterile environments, or pills that release medicine slowly over 12 hours. These are called complex generics. They require advanced formulation science, specialized equipment, and deep regulatory knowledge. There are fewer manufacturers who can make them. That means less competition. And that means better margins-sometimes 40-50%. Teva, once a commodity giant, now earns nearly half its revenue from these harder-to-make drugs. Lenalidomide for multiple myeloma? Austedo XR for movement disorders? These aren’t just generics. They’re engineered solutions with technical barriers that keep others out. Viatris, formed from the merger of Mylan and Upjohn, also shifted away from low-margin products. They sold off their OTC and API businesses to focus on what they could control: specialty generics and complex formulations. Their profit margin in 2025? 4.3%. Not huge, but stable. And they’re not losing money like Teva did. The FDA recognizes this trend. In 2024, they fast-tracked 37 complex generic applications. That’s up 40% from 2020. Companies that invest in R&D for these products aren’t just surviving-they’re building moats around their business.The Rise of Contract Manufacturing
What if you didn’t have to own the brand? What if you just made the drug for someone else? That’s the contract manufacturing model. Companies like Egis Pharma Services, founded in late 2023, now offer end-to-end production for branded and generic firms. They handle API synthesis, formulation, packaging, and regulatory filings-all under one roof. The client gets the product. The manufacturer gets the fee. This segment is growing fast. It’s projected to hit $90.95 billion by 2030, up from $56.53 billion in 2025. Why? Because big pharma doesn’t want to run factories anymore. They want to focus on R&D and marketing. Meanwhile, generic manufacturers with excess capacity see an opportunity to turn their plants into profit centers. This model also reduces risk. No need to fight for formulary placement. No need to negotiate with pharmacy benefit managers. You’re paid per unit, regardless of market price swings. For manufacturers in Europe or India, where labor and infrastructure costs are lower, this is a goldmine. Even companies like Teva are moving into this space. Their new strategy isn’t just about selling more drugs-it’s about becoming the go-to maker for others. It’s a quiet revolution: from brand competitor to service provider.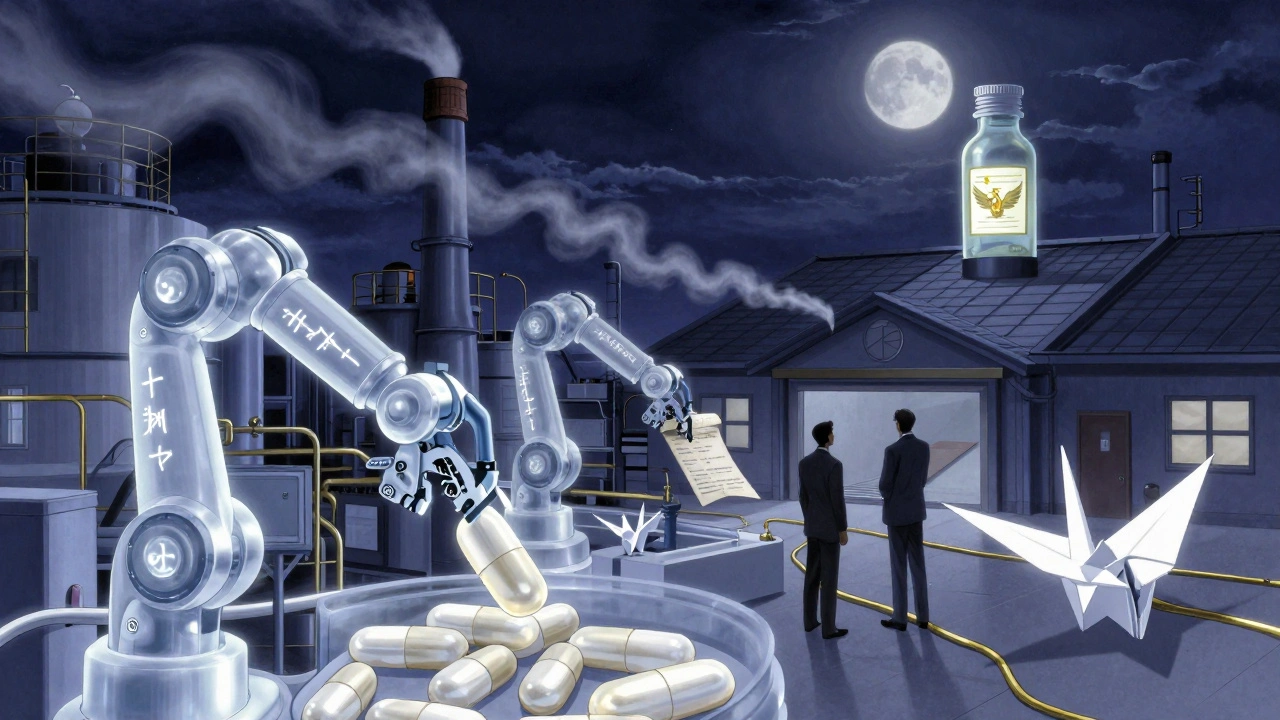
Why the U.S. Market Is Broken
The U.S. is the world’s largest market for generics-but also the most broken. Why? Pharmacy Benefit Managers (PBMs). These middlemen negotiate drug prices between insurers and pharmacies. But they don’t always pass savings to patients. Instead, they take rebates from manufacturers based on list prices. The lower the manufacturer’s price, the less rebate they get. So manufacturers are stuck: lower prices mean less revenue, but higher prices mean losing shelf space. This system rewards volume, not value. It punishes innovation. And it creates perverse incentives. One study estimated that banning “pay-for-delay” deals-where brand companies pay generics to stay off the market-could save $45 billion over ten years. But those deals still happen. And they keep prices artificially high, even as manufacturers struggle to make a profit. Meanwhile, the FDA’s approval process is slow. It takes 18-24 months just to get a new generic on the market. By then, the window for profit is shrinking. And with over 16,000 generic drugs already approved, the market is saturated.Global Differences Matter
Profitability isn’t the same everywhere. In Europe, government pricing systems set limits-but they also guarantee volume. Manufacturers know they’ll sell X amount at Y price. No wild swings. No PBM games. Margins are lower than in the U.S. pre-2010, but they’re stable. In India and China, manufacturers benefit from lower labor costs, strong chemical infrastructure, and government support. They dominate the global supply of APIs. But they face their own risks: currency fluctuations, environmental regulations, and political pressure to keep prices low. Emerging markets like Brazil, Indonesia, and Nigeria are growing fast. Demand for affordable drugs is rising. But infrastructure is weak. Distribution is unreliable. And regulatory systems are inconsistent. It’s a gamble: big potential, but high risk.
Sustainability Isn’t About Profit Alone
The real issue isn’t whether generic manufacturers can make money. It’s whether they can make enough to keep producing essential medicines. Dr. Aaron Kesselheim from Harvard put it bluntly: “The relentless price competition has created a market failure.” We’ve seen shortages of antibiotics, cancer drugs, and even insulin generics because no one could profitably make them. That’s not a business problem. It’s a public health crisis. The solution isn’t to raise prices for patients. It’s to redesign the system. Reward complexity. Protect innovation. Stop punishing manufacturers for being efficient. Pay for quality, not just cost. The future belongs to companies that move beyond commodity production. Those that build technical expertise. Those that partner with brands instead of fighting them. Those that invest in supply chain resilience. The global generic market will hit $600 billion by 2033. That’s not a fantasy. It’s based on over 50 blockbuster drugs set to lose patent protection between now and then. But if the business models don’t change, that growth won’t reach patients. It’ll just line the pockets of middlemen and leave manufacturers behind.What’s Next for Generic Manufacturers?
If you’re a generic manufacturer today, you have three choices:- Stay in commodity generics-and risk losing money or going out of business.
- Invest in complex generics, build technical expertise, and target niche markets with higher margins.
- Become a contract manufacturer, offering production services to others and reducing your exposure to price wars.
Why are generic drug profits falling despite high demand?
Demand for generics is high, but so is competition. When multiple manufacturers make the same simple drug, prices drop rapidly. Gross margins have fallen from 50-60% a decade ago to under 30% today. High fixed costs-like FDA approval fees and manufacturing facilities-mean companies can’t profit when prices crash. Many are losing money just to stay in the game.
What’s the difference between commodity and complex generics?
Commodity generics are simple, off-patent drugs like metformin or ibuprofen-easy to copy, made by dozens of companies, and sold at rock-bottom prices. Complex generics involve difficult formulations-like inhalers, injectables, or extended-release pills-that require advanced science and specialized equipment. Fewer companies can make them, so competition is lower and margins are higher-often 40-50%.
How do contract manufacturers make money in this industry?
Contract manufacturers don’t sell drugs under their own brand. Instead, they produce drugs for other companies-branded or generic-for a fee. This removes the risk of price wars and formulary battles. They get paid per unit, regardless of market conditions. This model is growing fast, with the global contract manufacturing segment expected to reach $90.95 billion by 2030.
Why is the U.S. generic market different from Europe’s?
In the U.S., Pharmacy Benefit Managers (PBMs) control pricing through rebates based on list prices, creating perverse incentives that punish low pricing. In Europe, governments set fixed prices and guarantee volume. While margins are lower, they’re stable. European manufacturers aren’t caught in the same price wars, so profitability is more predictable.
Are generic drug shortages linked to profitability?
Yes. When a drug’s price drops below the cost to make it, manufacturers stop producing it. This happens often with older, low-margin generics like antibiotics or chemotherapy drugs. The result? Shortages. Experts say this isn’t a supply chain issue-it’s a pricing failure. If manufacturers can’t profit, they won’t make the drug, even if it’s essential.
Will the generic drug market grow in the next decade?
Yes, but not in the way most people think. The traditional U.S. commodity generic market is shrinking. But the global market is projected to hit $600 billion by 2033, driven by patent expirations on major drugs, rising demand in emerging markets, and growth in complex generics and contract manufacturing. The winners will be those who move beyond low-cost, high-volume production.




Jimmy Kärnfeldt
December 12, 2025 AT 04:12It’s wild how we treat life-saving meds like commodities. You wouldn’t expect a firefighter to work for free just because the job is ‘essential.’ Yet we act like drug makers should bleed money just because people need their pills. We’re not fixing the system-we’re just blaming the makers while PBMs get richer. 🤷♂️
Ariel Nichole
December 14, 2025 AT 02:24I’ve been on metformin for years and pay like $4 a month. It’s insane that the company making it loses money on it. Maybe we need a ‘fair price’ model-not the lowest, but the one that keeps factories running. Everyone wins if the drug doesn’t disappear.
john damon
December 15, 2025 AT 21:42Bro… why is this so complicated?? 😅 Just pay people more. Or tax Big Pharma. Or something. I just want my insulin to not cost $300. 🤯
Taylor Dressler
December 16, 2025 AT 06:51The shift to complex generics and contract manufacturing is the only sustainable path forward. The low-margin commodity model is a dead end-it’s not a failure of innovation, it’s a failure of market design. We need policy that rewards technical capability, not just cost-cutting. The FDA’s fast-tracking of complex generics is a step in the right direction, but it needs to be systemic, not sporadic.
Sylvia Frenzel
December 17, 2025 AT 22:41U.S. manufacturers are weak. In China, they make 80% of the world’s APIs and still turn a profit. We’re letting our industry die because we can’t handle competition. Fix the system? Nah. Just outsource it and stop pretending we care.
Courtney Blake
December 18, 2025 AT 06:20Oh wow, another article about how drug companies are ‘struggling.’ Meanwhile, I’m choosing between my blood pressure med and groceries. Maybe if you stopped lobbying to keep prices high, you wouldn’t be losing money. This isn’t a tragedy-it’s karma.
Lisa Stringfellow
December 19, 2025 AT 05:30They’re not losing money. They’re just not making *enough*. And guess who pays the price? Us. The real tragedy isn’t the profit margin-it’s that we’ve normalized this. People die because a company decided a $0.02 pill isn’t worth the cost. This isn’t capitalism. It’s cruelty dressed up as economics.
Kristi Pope
December 19, 2025 AT 11:45Imagine if we treated hospitals like we treat car factories-where the only thing that matters is how cheap you can make a spark plug. We’d all be dead. Generic drugs aren’t widgets. They’re lifelines. And if we keep treating them like discount toilet paper, we’ll run out when we need them most. Let’s stop pretending this is just a business problem.
matthew dendle
December 21, 2025 AT 05:05so like… we pay 10x for brand names but then act shocked when the generics go broke? lol. someone get this guy a calculator. also pbms are the real villains. they’re the ones hoarding the cash while the makers starve. 🤡
Monica Evan
December 22, 2025 AT 09:41My cousin works at a generic plant in Ohio. They used to make 20 drugs. Now it’s three. The rest got shut down because the price dropped to 2 cents a pill. The workers aren’t rich, but they’re not poor either-until the plant closes. This isn’t about greed. It’s about survival. We need to pay for quality, not just cheapness. Simple as that.
Jean Claude de La Ronde
December 22, 2025 AT 19:28Canada’s system ain’t perfect but at least we don’t have PBMs playing 4D chess with our prescriptions. Here, the government sets a price, you make it, you get paid. No drama. No rebates. No ‘oh wait we’re losing money so we’re stopping production.’ Maybe if the U.S. stopped pretending it’s a free market and started acting like a country with a healthcare system, this wouldn’t be a problem.