
SSRI/SNRI Discontinuation Timeline Calculator
Medication Selection
Stopping an SSRI or SNRI isn’t like turning off a light switch. For many people, it’s more like slowly dimming a bulb that’s been on for years-except the dimming can cause strange, unsettling side effects that feel like the original illness is coming back. That’s not relapse. It’s discontinuation syndrome. And if you’re planning to stop, knowing what to expect can save you from unnecessary panic, misdiagnosis, or even a return to medication you didn’t want to restart.
Why Symptoms Show Up When You Stop
Your brain adapts to antidepressants. Over weeks or months, it changes how it produces, releases, and reabsorbs serotonin-and in the case of SNRIs, norepinephrine too. When you suddenly stop, those adjustments don’t reverse instantly. The neurotransmitters drop fast, but your brain hasn’t had time to recalibrate. That mismatch is what causes withdrawal symptoms. The timing of those symptoms depends almost entirely on how long the drug stays in your system. That’s measured by its half-life-the time it takes for half the drug to leave your body. For example, paroxetine (Paxil) has a half-life of about 24 hours. That means within a day or two of missing a dose, your blood levels drop sharply. Symptoms often start within 1-3 days. Venlafaxine (Effexor), with a 5-hour half-life, can trigger symptoms in under 24 hours. On the other end, fluoxetine (Prozac) lingers for days-sometimes up to six. Its effects fade slowly, so withdrawal symptoms might not show up for weeks, or even months. This isn’t just academic. Getting the timing wrong can make you think your depression is returning when it’s really your brain adjusting. Studies show up to 30% of people who stop too quickly are misdiagnosed with relapse, leading to unnecessary restarts.How Long Do Symptoms Last?
Most people experience symptoms for 1-2 weeks. That’s what most clinical guidelines say. But real-world experience tells a different story. A 2023 survey of over 15,000 people in the Reddit r/antidepressants community found that 68% had symptoms lasting longer than two weeks. Nearly half said they lasted months. One person, who tapered paroxetine over six months, still had brain zaps and dizziness at 11 months. That’s not rare. A 2019 Lancet Psychiatry study found 46% of people needed more than six months to fully stop. The truth? While 80% of symptoms fade within two weeks, 10-20% of people deal with lingering issues-brain zaps, insomnia, nausea, anxiety-for months. These are called protracted withdrawal. It’s not well understood, but it’s real. And it’s why many experts now say: slow is safer than fast.Medication-Specific Timelines
Not all antidepressants are created equal when it comes to stopping. Here’s what you can expect based on the drug you’re on:- Paroxetine (Paxil): Fastest onset. Symptoms in 1-3 days. Hardest to stop. High risk of dizziness, nausea, and electric shock sensations.
- Sertraline (Zoloft): Half-life around 26 hours. Symptoms in 1-3 days. Moderate severity.
- Escitalopram (Lexapro): Half-life 27-32 hours. Symptoms start in 2-4 days. Generally milder than paroxetine.
- Citalopram (Celexa): Half-life 36 hours. Symptoms appear around day 3-4.
- Fluoxetine (Prozac): Half-life 4-6 days. Symptoms may not appear for weeks. Can be easier to taper, but requires 3-month monitoring for late-emerging effects.
- Venlafaxine (Effexor): Half-life 5 hours. Symptoms in 24-48 hours. Highest rate of severe symptoms-78% report dizziness, 62% report brain zaps.
- Duloxetine (Cymbalta) and Desvenlafaxine (Pristiq): Half-life around 12 hours. Symptoms in 1-3 days. Often more intense than SSRIs.
SNRIs, especially venlafaxine, tend to cause worse symptoms than SSRIs. That’s why many doctors recommend switching to fluoxetine before tapering if you’re on venlafaxine-it gives your brain a buffer.

Tapering: The Real Debate
Here’s where things get messy. Clinical guidelines disagree wildly. Some say: taper over 2-4 weeks. Reduce by 25% every week. Done. Others-especially those who’ve seen patients suffer-say: take 6-12 months. Reduce by 10% per step. Wait 4-8 weeks between each drop. Let your body catch up. The NSW Therapeutic Advisory Group suggests reducing by 25% every 1-4 weeks, then slowing to 12.5% at the end. The British Association of Psychopharmacology admits there’s no solid evidence for any specific rate. The 1997 Stanford consensus panel said taper all antidepressants except fluoxetine. Why the chaos? Because we don’t have enough high-quality studies. Most trials are short. They measure relapse, not withdrawal. And they rarely follow patients long enough to see what happens after 3 months. The real answer? It’s not about the calendar. It’s about your symptoms. Dr. Mark Horowitz, who led a major 2019 review, says: “Tapering should be driven by patient symptoms, not arbitrary percentages.” If you feel dizzy, nauseous, or anxious after a reduction, stop. Stay at that dose. Wait. Your brain needs time.What to Do If Symptoms Hit
If you start feeling off during a taper:- Don’t panic. It’s likely withdrawal, not relapse.
- Hold your current dose. Don’t go lower.
- Wait 1-2 weeks. Most symptoms fade in that time.
- If they don’t, go back up to your last stable dose and try a slower taper next time.
- Severe symptoms like suicidal thoughts, extreme anxiety, or seizures? Contact your doctor immediately.
Restarting your original dose-even briefly-usually stops symptoms within 24 hours. That’s a key clue: if you feel better after restarting, it was withdrawal, not depression returning.
Practical Tips for Safer Stopping
- Never stop cold turkey. Even if you feel fine, your brain isn’t ready. - Use liquid formulations if possible. They allow for tiny, precise reductions-down to 1-2.5% at a time. A 2023 University of Toronto study showed this cuts severe symptoms by 63%. - Avoid generic switches. Switching from brand to generic or between generics can cause a 20% drop in blood levels-mimicking abrupt withdrawal. - Work with someone experienced. A 2023 Cleveland Clinic study found 92% of successful discontinuations happened with providers trained in tapering. Only 47% succeeded with general practitioners. - Track your symptoms. Use a journal. Note mood, sleep, dizziness, brain zaps, nausea. Patterns help you and your doctor adjust. - Be patient with fluoxetine. Even though it’s easier to taper, symptoms can appear months later. Monitor for at least 12 weeks after your last dose.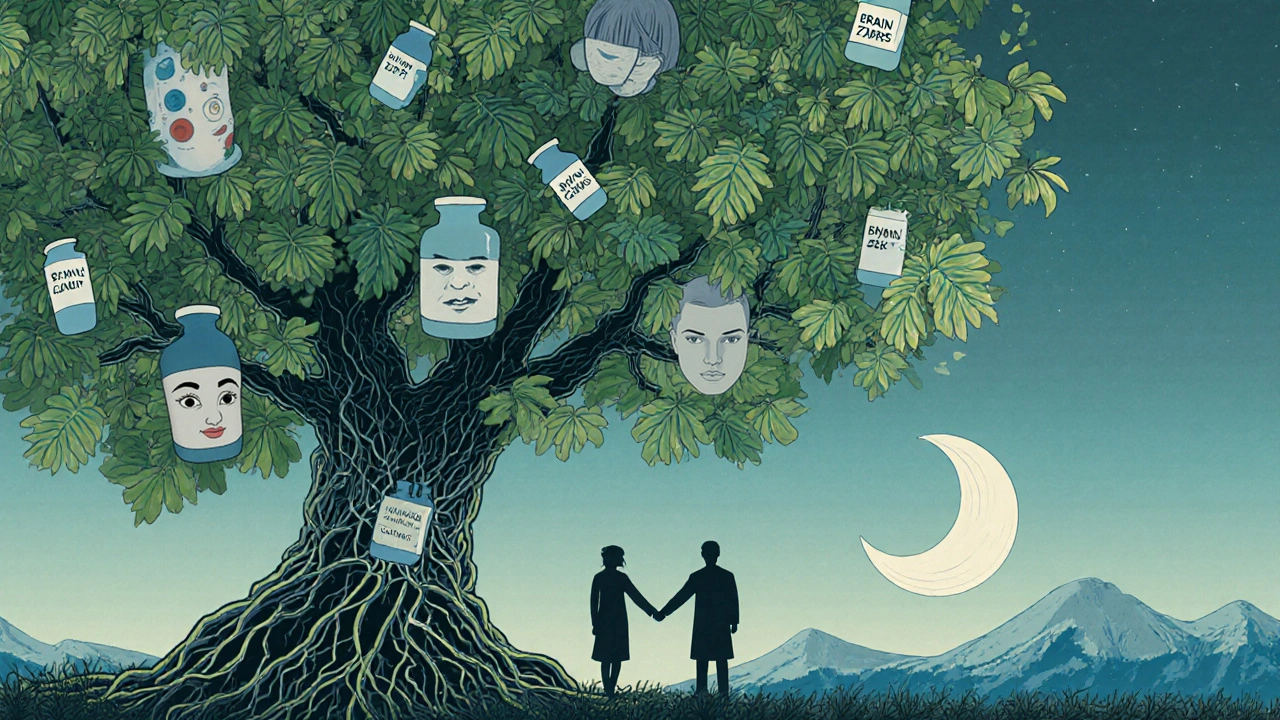
When to Get Help
Some symptoms are red flags:- Suicidal thoughts (reported in 4.2% of discontinuation attempts)
- Severe anxiety or panic attacks (28.7% of cases)
- Neurological symptoms like seizures, loss of coordination, or persistent brain zaps (63.1%)
- High fever, rapid heartbeat, or confusion (signs of serotonin syndrome)
If you experience any of these, contact your doctor immediately. Don’t wait. These aren’t normal withdrawal effects-they need medical attention.
The Bigger Picture
Right now, most doctors still recommend tapers under 4 weeks. But a 2023 British Medical Journal study found 68% of people who stopped in under 8 weeks had relapse or severe withdrawal. Only 22% did when tapers lasted over 20 weeks. The FDA now requires updated medication guides that include individualized tapering advice. The American Psychiatric Association is updating its guidelines in 2024 to include patient-reported outcomes. The European Medicines Agency says current guidelines fail 40-60% of patients. This isn’t just about pills. It’s about listening to people who’ve lived through it. The data from Reddit, Surviving Antidepressants, and patient surveys is now shaping real policy changes. You’re not broken if you need months to stop. You’re not weak if you need help. You’re just human.What Comes Next
If you’re thinking about stopping, start by talking to your prescriber. Ask:- What’s the half-life of my medication?
- Do you have experience helping patients taper?
- Can we use a liquid form or compounding pharmacy for smaller doses?
- How will we monitor symptoms?
- What’s the plan if I feel worse?
There’s no one-size-fits-all timeline. But there is a better way: slow, informed, symptom-driven, and patient-centered. The goal isn’t just to stop the drug. It’s to stop it without losing your health along the way.




Julie Pulvino
November 24, 2025 AT 06:30Wow, this is the most clear-headed guide I’ve read on this topic. I tapered off sertraline over 8 months and still got brain zaps at 7 months-felt like my head was doing cartwheels. Everyone told me I was ‘overreacting.’ Turns out, I wasn’t.
Thanks for laying this out so plainly. This should be mandatory reading for every prescriber.
Patrick Marsh
November 25, 2025 AT 01:42Never cold-turkey. Ever. I did it once. Regretted it for a year.
David Cunningham
November 26, 2025 AT 05:38Been through this twice. First time with venlafaxine-holy hell. Second time with fluoxetine, switched to liquid, dropped 1% every 3 weeks. Took 14 months. Felt like a snail. But I’m finally me again. No zaps. No nausea. Just quiet.
Slow is the only way.
Nikhil Chaurasia
November 27, 2025 AT 15:51My doctor told me to cut my dose in half over two weeks. I did. Three days later, I was crying in the grocery store for no reason. He said, ‘Maybe your depression’s back.’
No. It was my brain screaming for mercy. I went back up. Now I’m tapering slow, with a journal, and I’m actually healing-not just surviving.
Danny Nicholls
November 29, 2025 AT 14:13Guys. Liquid formulations are a game-changer. Seriously. I was on 25mg of citalopram and needed to drop to 18mg. No pills existed. Compounded pharmacy did it for $15. Took me 10 months to get off. No brain zaps. No panic.
Also, if you’re using generics, check the manufacturer. One batch felt like I’d been hit by a truck. Switched back to brand. Instant relief. Don’t let big pharma mess with your brain chemistry without telling you.
Also, if you’re feeling weird after a switch-stop. Don’t push through. Your brain isn’t a car engine.
Also, keep a journal. Write down your zaps. Date them. It helps. Trust me.
Also, you’re not weak. You’re human.
Also, I cried at a Taco Bell once. It was fine.
Also, emojis are valid. 🙃
Daniel Jean-Baptiste
November 29, 2025 AT 19:14Had a friend taper off paroxetine in 3 weeks. Ended up in the ER with serotonin syndrome. They didn’t even know it was withdrawal.
Doctors need to stop treating this like a checklist. This isn’t a math problem. It’s a biological recalibration. Your brain isn’t a light switch. It’s a garden. You don’t yank the roots. You prune slowly, with care.
Also, Reddit data is legit. We’re the real-world lab.
And yes, fluoxetine’s long half-life is a blessing. But don’t get lazy. Still monitor for months. I didn’t. Got zaps at 5 months. Felt like a ghost in my own head.
Rahul Kanakarajan
December 1, 2025 AT 10:56Everyone’s making this sound like a trauma. It’s just a drug. You took it. Now you’re done. Stop whining. Just go cold turkey. You’ll be fine. It’s all in your head anyway.
Also, why are you on antidepressants in the first place? Maybe you just need to exercise more. Or pray. Or get a job. Or stop being so sensitive.
Also, I’ve never taken one. But I know better.
New Yorkers
December 2, 2025 AT 15:41The real tragedy isn’t the withdrawal.
It’s that we’ve turned healing into a corporate algorithm.
Doctors follow guidelines written by committees who’ve never felt a brain zap.
We’ve commodified the soul’s quiet rebellion against chemical calm.
You don’t taper off an antidepressant.
You re-emerge from a borrowed identity.
And the system? It doesn’t want you to remember who you were before the pills.
So it tells you to go slow.
But slow is just another cage.
…or maybe I’m just overthinking it.
Probably am.
Anyway, I’m off my meds now.
And I feel… nothing.
And that’s the point.
Robin Johnson
December 2, 2025 AT 16:34For anyone thinking about stopping: start by talking to your doctor before you even think about reducing. Don’t wait until you’re in crisis.
Find someone who’s done this before. Ask for liquid. Ask for a journal. Ask for patience.
You’re not failing if it takes months. You’re succeeding if you’re still here, still trying.
And if you slip up? That’s okay. You don’t have to be perfect. You just have to be persistent.
I’m 11 months out. Still get the occasional dizziness. But I’m living. Not just surviving.
You got this.
luke young
December 3, 2025 AT 21:04Just wanted to say thank you for this. I’m 6 months into my taper and I’ve been terrified every step of the way. This post made me feel less alone.
Also, I started using a mood tracker app. It’s dumb, but seeing the dips and rises helped me realize my ‘relapse’ was just a wave. It passed.
Keep going. You’re doing better than you think.
Julie Pulvino
December 3, 2025 AT 23:09Thank you for sharing that. I didn’t know others felt the same way about the app. I’ve been using Daylio too. It’s wild how much clearer the pattern looks when you write it down.
Also, I cried reading your comment. Not because I’m sad. Because I finally feel seen.