Enlarged Prostate Hormone Therapy Calculator
Estimate Prostate Volume Reduction
Select your treatment option and enter your prostate volume to see estimated benefits.
Estimated Results
Important Information
This calculator provides an estimate based on clinical data. Actual outcomes may vary depending on individual patient factors.
Always consult with a healthcare provider for personalized treatment recommendations.
When doctors talk about hormone therapy is a treatment that modifies hormone levels to influence prostate tissue growth, they’re exploring a strategy that’s gaining traction for the enlarged prostate. Men over 50 often notice a slow‑growing, non‑cancerous swelling called Benign Prostatic Hyperplasia (BPH), which can make urinating difficult and affect quality of life. This article breaks down why hormone‑based approaches work, how they compare with other options, and what patients should watch out for.
What Exactly Is an Enlarged Prostate?
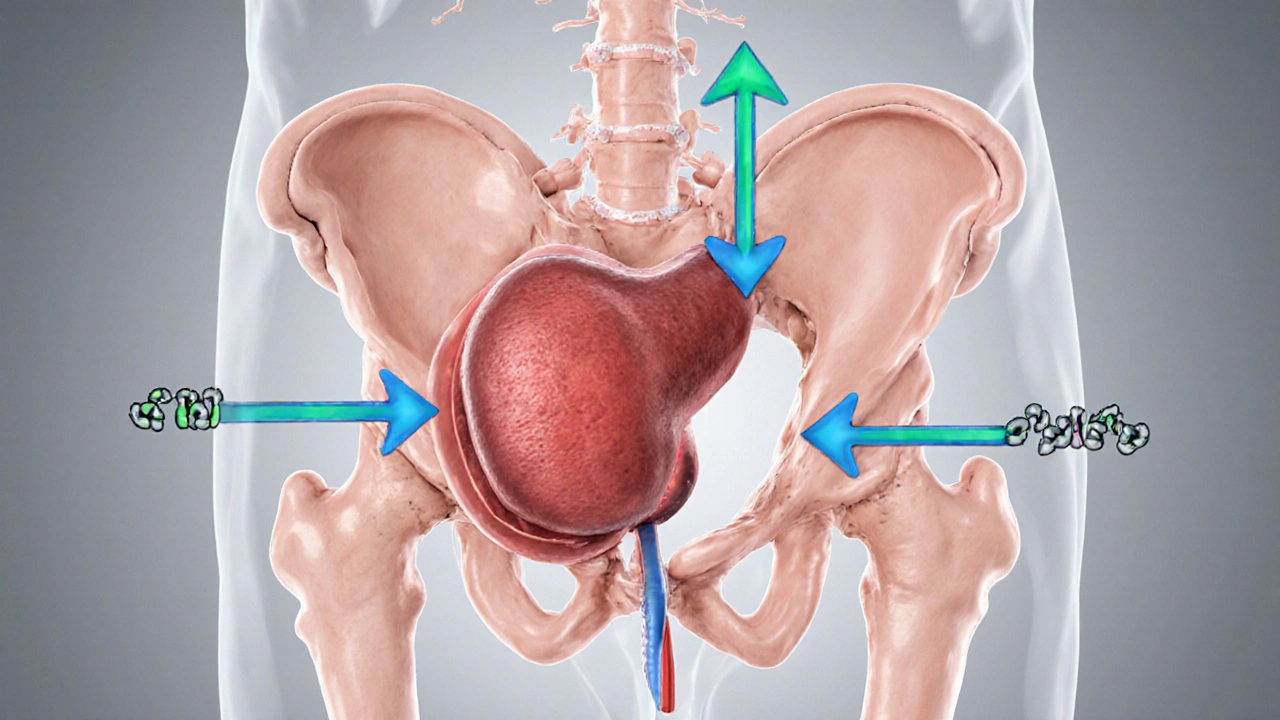
BPH is a benign increase in prostate size caused by hormonal changes, especially the rise of testosterone and its more potent derivative dihydrotestosterone (DHT). As the gland expands, it squeezes the urethra, leading to lower urinary tract symptoms (LUTS) such as frequent nighttime trips, weak stream, and urgency. While the condition isn’t life‑threatening, the discomfort can be significant.
How Hormones Drive Prostate Growth
The prostate depends on androgens for development and maintenance. Testosterone is converted to DHT by the enzyme 5‑alpha‑reductase. DHT binds tightly to androgen receptors in prostate cells, prompting them to multiply. Over time, the cumulative effect of this signaling leads to the nodular growth seen in BPH. Reducing either testosterone levels or DHT activity can therefore slow or even reverse enlargement.

Hormone‑Based Therapies Used in BPH
Several hormone‑modulating drugs have been repurposed from prostate‑cancer treatment to address BPH:
- 5‑alpha‑reductase inhibitors (5‑ARIs) - Medications such as finasteride and dutasteride block the enzyme that makes DHT, lowering its concentration by up to 70%.
- Androgen deprivation therapy (ADT) - Drugs like goserelin (a GnRH agonist) suppress testicular testosterone production, creating a low‑androgen environment.
- Selective estrogen receptor modulators (SERMs) - While less common, agents like tamoxifen have shown modest prostate‑size reduction in early trials.
Each approach targets a different step in the androgen pathway, allowing clinicians to tailor treatment based on patient age, symptom severity, and co‑existing conditions.
Clinical Evidence: Does Hormone Therapy Actually Shrink the Prostate?
Large, randomized trials have examined 5‑ARIs for BPH. The landmark Prostate Cancer Prevention Trial (PCPT) reported a 25% reduction in prostate volume after five years of finasteride, accompanied by a 30% drop in LUTS scores. The Combination of Avodart and Tamsulosin (CAM) study showed that adding dutasteride to an alpha‑blocker cut urinary symptom scores by an extra 10 points versus alpha‑blocker alone.
ADT is more aggressive. A 2022 multi‑center study of men with severe BPH who were unsuitable for surgery found that a six‑month course of goserelin reduced prostate volume by 20% and improved peak urinary flow by 4mL/s. However, side‑effects such as hot flashes and loss of bone density limited long‑term use.
Overall, hormone therapy works best when combined with symptom‑relief drugs (alpha blockers) or when surgery is high‑risk. It offers a non‑invasive way to address the root cause-excess androgen signaling.
How Hormone Therapy Stacks Up Against Other BPH Options
| Treatment | Mechanism | Typical Volume Reduction | Side‑Effect Profile | Best For |
|---|---|---|---|---|
| Alpha blockers | Relax smooth muscle in prostate and bladder neck | ≈0% (symptom‑only) | Dizziness, low blood pressure | Men with mild‑moderate LUTS |
| 5‑alpha‑reductase inhibitors | Block conversion of testosterone to DHT | 20‑30% reduction over 2‑5years | Sexual dysfunction, breast tenderness | Men with larger prostates (>40mL) |
| Androgen deprivation therapy | Suppress overall testosterone production | ≈20% in 6months | Hot flashes, bone loss, metabolic changes | High‑risk patients unsuitable for surgery |
| Surgical interventions (TURP) | Physically remove prostate tissue | ≈70‑80% immediate relief | Bleeding, urinary incontinence, erectile issues | Severe obstruction or failed medical therapy |
The table highlights that hormone therapy sits between simple symptom control and invasive surgery. It offers measurable shrinkage without the risks of an operation, but it does carry hormonal side‑effects that need monitoring.

Benefits, Risks, and Who Should Consider Hormone Therapy
Benefits include:
- Actual reduction in prostate size, not just symptom masking.
- Potential to delay or avoid surgery.
- Improved flow rates and reduced nighttime trips.
Risks vary by drug class:
- 5‑ARIs may cause libido loss, erectile dysfunction, and rare cases of high‑grade prostate cancer.
- ADT can lead to osteoporosis, metabolic syndrome, and cardiovascular strain.
Ideal candidates are men with:
- Prostate volume >40mL (where 5‑ARIs show the most impact).
- Moderate to severe LUTS not fully controlled by alpha blockers.
- Contraindications to surgery or a strong desire to avoid it.
Baseline labs-PSA, testosterone, liver function-and a bone‑density scan (for ADT) are essential before starting therapy.
Practical Checklist for Patients Starting Hormone Therapy
- Schedule a comprehensive urologic exam, including prostate ultrasound to measure volume.
- Get baseline blood work: PSA, total testosterone, liver enzymes, lipid profile.
- Discuss lifestyle factors-exercise, calcium/vitamin D intake-to offset bone‑loss risk.
- Choose the hormone agent (5‑ARI vs ADT) based on prostate size, symptom severity, and comorbidities.
- Set follow‑up intervals: PSA and prostate volume every 6months for the first year.
- Monitor side‑effects: sexual function, mood changes, blood pressure, bone health.
- Re‑evaluate after 12months-if volume reduction <15% or symptoms unchanged, consider adding an alpha blocker or discussing surgical options.
Sticking to this checklist helps maximize benefits while catching problems early.
Frequently Asked Questions
Can hormone therapy cure BPH?
It doesn’t cure the condition, but it can shrink the prostate and significantly improve urinary symptoms, often postponing the need for surgery.
How long do I need to stay on a 5‑alpha‑reductase inhibitor?
Most guidelines suggest at least 6months to see a meaningful volume reduction, and many men stay on the drug indefinitely if it continues to help.
Are there any natural ways to lower DHT?
Lifestyle measures-maintaining healthy weight, reducing alcohol, and eating foods rich in zinc and lycopene-may modestly lower DHT, but they’re not a substitute for prescription therapy when significant prostate reduction is needed.
What’s the biggest drawback of androgen deprivation therapy for BPH?
Systemic suppression of testosterone can cause hot flashes, loss of bone density, and changes in metabolism, making it a less popular choice unless surgery is off‑limits.
Do I need regular PSA testing while on hormone therapy?
Yes. Hormone therapy can lower PSA, but rising levels may still signal cancer, so clinicians monitor PSA trends every 6-12months.




Ujjwal prakash
October 6, 2025 AT 13:52Hormone therapy for BPH is not just a trendy buzzword, it’s a clinically validated approach, especially when you consider the 5‑alpha‑reductase inhibitors that have shown a 20‑30% reduction in prostate volume over several years, and that’s after you factor in patient compliance, side‑effect profiles, and real‑world outcomes, which are often overlooked in marketing hype, so don’t be fooled by the superficial hype; dive into the data and you’ll see why many urologists prefer a combined regimen.
Diane Helene Lalande
October 8, 2025 AT 21:25Great overview, thanks for sharing the details.
Edwin Levita
October 10, 2025 AT 23:25Ah, the drama of hormonal manipulation! One cannot simply reduce a prostate without contemplating the existential weight of diminishing a gland that, for centuries, has been a silent sentinel of masculinity. The interplay of testosterone and DHT is nothing short of a tragic opera, each molecule singing its own aria of proliferation. Yet, the modern pharmacopeia-finasteride, dutasteride-offers a deus ex machina, whispering promises of volume reduction while courting side‑effects like a lover with a hidden agenda. One must ask: are we tampering with nature or merely correcting an overzealous evolutionary quirk? The answer lies in the patient’s narrative, not merely in the numbers on a chart. In any case, the theater of BPH treatment continues, lights dimming on the old and shining on the new.
Xander Laframboise
October 12, 2025 AT 19:52While the article paints hormone therapy in a rosy light, remember that long‑term androgen suppression can aggravate metabolic syndrome, increase cardiovascular risk, and even affect cognitive function. Not every patient tolerates a 20% volume reduction if it comes at the cost of quality of life elsewhere. So, weigh the benefits against the systemic repercussions before opting for ADT as a first‑line strategy.
Jason Petersen
October 14, 2025 AT 13:32Too many pills, not enough results.
Melissa Gerard
October 16, 2025 AT 04:25Looks like another pharma push 🤔
Cindy Knox
October 17, 2025 AT 16:32Thanks for the clear breakdown! This helps a lot.
beverly judge
October 19, 2025 AT 01:52For anyone starting 5‑ARI therapy, remember to schedule a PSA check at baseline and then every 6 months. Also, consider a bone‑density scan if you’re leaning toward ADT, as the risk of osteoporosis rises. Lastly, maintain a healthy diet rich in calcium and vitamin D to mitigate bone loss.
Capt Jack Sparrow
October 19, 2025 AT 01:52The data from the PCPT and CAM studies clearly demonstrate that 5‑ARIs reduce prostate volume by roughly a quarter over multiple years. When combined with an alpha‑blocker, patients often see additive symptom improvement. However, the onset of volume reduction can be slow, taking up to 3–5 years to reach full effect. ADT, on the other hand, offers a more rapid decline but at the expense of systemic hormonal changes. Clinicians must balance urgency of symptom relief with tolerability of side‑effects.
Manju priya
October 20, 2025 AT 08:25Stay motivated to follow up regularly; consistent monitoring can make a huge difference in outcomes. 😊
Jesse Groenendaal
October 21, 2025 AT 12:12We must not forget the moral responsibility to inform patients fully about potential sexual side‑effects; ignorance is no excuse.
Persephone McNair
October 22, 2025 AT 13:12From a pathophysiological standpoint, the androgen axis modulates stromal‑epithelial interactions, thereby influencing hyperplastic nodular formation. Inhibitors targeting 5‑alpha‑reductase attenuate this cascade, resulting in measurable volumetric decrement. Nonetheless, one must consider pharmacokinetic variability and receptor polymorphisms that may affect therapeutic efficacy. Clinical algorithms should integrate these molecular nuances for personalized therapy.
siddharth singh
October 23, 2025 AT 11:25When evaluating hormone therapy for BPH, the first step is a comprehensive urologic assessment, which includes a digital rectal exam (DRE) and transrectal ultrasound to quantify prostate volume accurately. Next, baseline labs are essential: PSA, total testosterone, liver function tests, and a complete metabolic panel to identify any contraindications. Patients should be educated about lifestyle modifications, such as reducing caffeine and alcohol intake, as these can exacerbate lower urinary tract symptoms. If the prostate volume exceeds 40 mL, a 5‑alpha‑reductase inhibitor (5‑ARI) becomes a strong candidate, given its proven efficacy in volume reduction over a multi‑year timeframe. For men with severe symptoms and a volume greater than 60 mL who are poor surgical candidates, androgen deprivation therapy (ADT) may be considered, but only after a thorough discussion of its systemic side‑effects, including hot flashes, loss of bone mineral density, and potential cardiovascular implications. During the first three months of therapy, patients should be monitored closely for any adverse reactions, and dosage adjustments made if necessary. It is also advisable to supplement calcium and vitamin D, especially when using ADT, to mitigate the risk of osteoporosis. Follow‑up imaging should be scheduled at six‑month intervals to assess changes in prostate size and correlate them with symptom improvement. If the volume reduction is inadequate or symptoms persist, combination therapy with an alpha‑blocker can be introduced to provide quicker symptomatic relief while the hormonal agent takes effect. Throughout the treatment course, open communication between the patient and the urologist is vital to ensure adherence, manage expectations, and promptly address any emerging concerns. Finally, after a year of stable improvement, clinicians can consider tapering the hormonal therapy, re‑evaluating the necessity of continued treatment based on ongoing symptomatology and prostate measurements. This systematic, patient‑centered approach maximizes therapeutic benefit while minimizing unnecessary exposure to medication side‑effects.
Angela Green
October 24, 2025 AT 06:52Just a quick note: “their” should be used instead of “there” in the sentence about “their side‑effects”. Also, “its” not “it’s” when referring to the therapy’s efficacy.
April Malley
October 24, 2025 AT 23:32Absolutely, the data is compelling, especially when you consider the long‑term reduction percentages, the improved quality of life metrics, and the decreased need for surgical interventions, which can be a huge relief for many patients.
scott bradshaw
October 25, 2025 AT 13:25Oh great, another excuse to medicate the masses.
Crystal Price
October 26, 2025 AT 00:32When we speak of shrinking a gland, we are really confronting the impermanence of the body itself, a reminder that even our most steadfast parts are subject to change.
Murhari Patil
October 26, 2025 AT 07:52The pharma giants don’t want you to know that these hormones are part of a larger agenda to control population health outcomes. Their silent experiments are hidden behind clinical trials, and the side‑effects are just the tip of the iceberg.
kevin joyce
October 26, 2025 AT 13:25From a mechanistic perspective, inhibiting 5‑alpha‑reductase alters the intracellular androgen milieu, which in turn modulates gene expression pathways governing cellular proliferation. This biochemical shift translates clinically into measurable reductions in prostate volume, albeit with a latency period reflective of tissue remodeling dynamics. It is crucial, however, to balance these benefits against the psychosocial impact of reduced libido and potential mood alterations, which patients often underreport. Integrating patient‑reported outcomes with objective metrics can guide personalized therapy adjustments, ensuring both efficacy and tolerability. Ultimately, the decision matrix should prioritize patient preference, comorbid conditions, and long‑term health trajectories.
michael henrique
October 26, 2025 AT 16:12Let’s be clear: this is not a choice for the average citizen, but a strategic move by our healthcare system to standardize treatment and cut costs. If you value your independence, push back against blanket prescriptions and demand individualized care.