
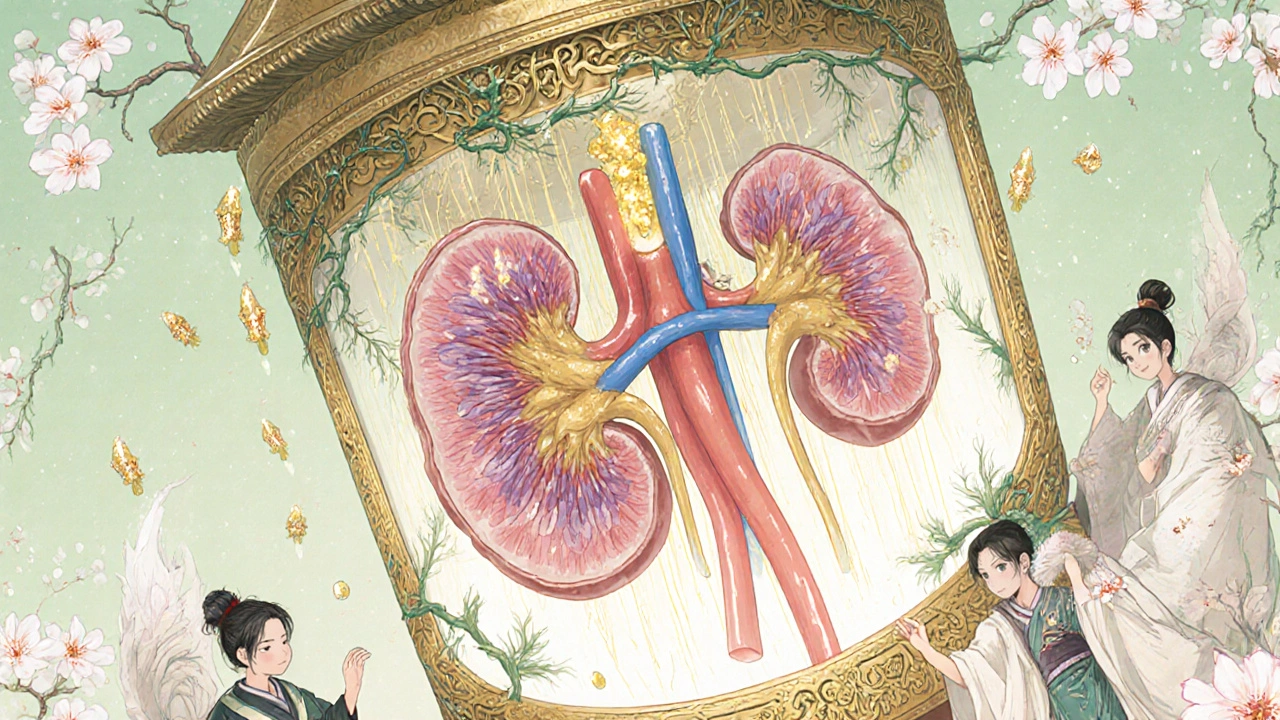
What Exactly Is Gout, and Why Does It Hurt So Much?
Gout isn’t just a bad joint ache. It’s a direct result of your body making too much uric acid-or not flushing it out well enough. When uric acid builds up, it forms sharp, needle-like crystals in your joints. These crystals trigger intense inflammation, swelling, and pain-often hitting the big toe first, but also ankles, knees, and fingers. This isn’t something that goes away on its own. Left untreated, gout can destroy joints and form visible lumps under the skin called tophi. And it’s not rare: over 8 million Americans live with it, and the numbers keep rising.
Why Do Uric Acid Levels Go Up? It’s All About Purines
Your body breaks down purines-natural substances found in your cells and in certain foods-to make uric acid. Humans lost the enzyme that turns uric acid into something harmless millions of years ago, so we’re stuck with it. About 65% of uric acid leaves your body through urine, and the rest through your gut. But here’s the problem: your kidneys reabsorb up to 90% of the uric acid they filter. That means even if you’re producing normal amounts, your body might still hold onto too much.
Purines come from two places: your own cells (about 80%) and what you eat (about 20%). High-purine foods like liver (240-400 mg per 100g), anchovies (500 mg per 100g), and beer (10-20 g per liter) can push levels higher. But diet alone rarely causes gout. The real issue is how your body handles purines internally. If enzymes like xanthine oxidase or URAT1 transporters are overactive, or if your kidneys can’t excrete properly, uric acid piles up.
What’s the Target? Lowering Uric Acid to Prevent Damage
Doctors don’t just want to stop a flare-they want to prevent long-term damage. The goal isn’t to get uric acid to normal. It’s to get it below the crystalization point. That’s 6.0 mg/dL for most people. If you have tophi or frequent flares, the target drops to 5.0 mg/dL. At levels above 9.0 mg/dL, more than a quarter of people will develop gout. At levels under 6.0 mg/dL, it’s less than 1%. That’s not a coincidence. Keeping uric acid low is the only proven way to dissolve crystals and stop gout from coming back.
The Three Types of Urate-Lowering Medications
There are three main classes of drugs that lower uric acid-and they work in completely different ways.
Xanthine Oxidase Inhibitors (XOIs): Stop Production at the Source
These drugs block xanthine oxidase, the enzyme that turns xanthine into uric acid. Allopurinol, approved in 1966, is the oldest and cheapest. Generic allopurinol costs about $4.27 a month. It’s the first choice for 85% of patients. But here’s the catch: most people take too little. The standard 100 mg dose rarely works. Doctors need to increase it slowly-by 100 mg every 2-5 weeks-until uric acid hits target. A 2023 study found 92% of patients reach their goal when dosed properly, often at 300 mg or higher.
Febuxostat, approved in 2009, is stronger and works even if your kidneys are weak. At 80 mg daily, it hits target in nearly 67% of patients. But it comes with a black box warning: a 2018 study showed it increased heart-related deaths compared to allopurinol. If you have heart disease, allopurinol is safer. If you can’t tolerate allopurinol, febuxostat is the next step.
Uricosurics: Help Your Kidneys Flush It Out
These drugs block URAT1, the main transporter that reabsorbs uric acid in your kidneys. Probenecid, approved in 1949, works well if your kidneys are healthy and you’re not dehydrated. But if your creatinine clearance is below 50 mL/min, it won’t help-and could even harm. It’s also less effective than XOIs. Lesinurad was approved in 2015 but pulled from the market in 2019 because it caused kidney damage. Newer drugs like verinurad are in late-stage trials and may offer safer options soon.
Uricase Therapy: Break Down Uric Acid Completely
Pegloticase is a biologic drug that turns uric acid into allantoin, a harmless substance your body easily flushes. It’s reserved for severe, tophaceous gout that hasn’t responded to anything else. In clinical trials, it dissolved tophi in 42% of patients within six months. But it’s expensive-$16,428.80 a month-and requires premedication to prevent severe allergic reactions. Many patients need 10-20 insurance appeals just to get it covered.
What Happens When You Start These Drugs?
Starting a urate-lowering medication doesn’t calm gout-it can make it worse. As crystals begin to dissolve, they trigger inflammation. That’s why doctors always prescribe colchicine (0.6 mg once or twice daily) for at least six months when starting treatment. Skipping this step leads to flares. One Reddit user wrote: “After six months on 300mg allopurinol, my uric acid dropped from 9.2 to 5.8-but I had three flares during titration. My doctor never warned me.” That’s not uncommon. Up to 61% of patients stop their meds within a year because they think the drug isn’t working. In reality, they’re just experiencing the side effect of healing.
Side Effects and Real-World Challenges
Allopurinol causes a rash in 42% of users. For 12%, it’s severe enough to require stopping the drug. That’s why some doctors test for HLA-B*58:01 gene before prescribing-it’s a strong predictor of serious reaction, especially in people of Asian descent. The FDA now requires this screening for pegloticase too.
Febuxostat can raise liver enzymes. About 31% of users need monitoring. And while it’s more effective than allopurinol, its cost is over 13 times higher. Many patients can’t afford it without insurance.
Pegloticase is the most effective but also the most complex. You get it via IV every two weeks. You need to be monitored for infusion reactions. And you need a battle plan for insurance. One patient said: “It changed my life. My tophi dissolved in nine months. But I had to fight my insurer 17 times.”
Diet and Lifestyle: Helpful, But Not Enough
Yes, cutting out organ meats, shellfish, and beer helps. Yes, losing weight and drinking more water lowers uric acid. But studies show diet alone typically drops levels by only 1-2 mg/dL. That’s not enough to reach the 6.0 mg/dL target for most people. Medication is still required. Diet is support-not a cure.

Why So Many People Fail to Control Gout
Despite clear guidelines, only 37% of gout patients in the U.S. reach their target uric acid level. Why? Three reasons: doctors don’t titrate doses enough, patients stop meds because of flares or side effects, and no one checks uric acid levels regularly. A 2024 study found only 29% of primary care doctors monitor uric acid every 2-5 weeks during dose escalation. Without that data, you’re flying blind.
What’s Coming Next?
Research is moving fast. Verinurad, a new uricosuric, is in Phase III trials and shows promise when paired with febuxostat. Arhalofenate, a drug that lowers uric acid and reduces inflammation at the same time, cut flare frequency by 58% in a 2024 trial. Scientists are also looking at genetic markers like SLC2A9 variants to predict who responds best to which drug. The goal: personalized gout treatment.
What You Need to Do Now
If you have gout, your job isn’t to wait for the next flare. It’s to get your uric acid below 6.0 mg/dL. Here’s your checklist:
- Ask your doctor for a serum uric acid test-don’t wait for pain.
- If your level is above 6.0 mg/dL, ask about starting allopurinol at 100 mg daily.
- Insist on dose titration: increase by 100 mg every 2-5 weeks until target is reached.
- Take colchicine daily for at least six months while starting treatment.
- Get your uric acid retested every 2-5 weeks during titration, then every 6 months after.
- If you get a rash or liver enzyme spike, don’t quit-talk to your rheumatologist. There are alternatives.
Gout is not a punishment for eating too much steak. It’s a metabolic disorder with a clear medical solution. The tools to fix it exist. What’s missing is consistent, guided treatment. Don’t let fear of side effects or confusion about dosing stop you. You can live without flares. You just need the right plan-and the right support.




Iska Ede
November 17, 2025 AT 08:03Gabriella Jayne Bosticco
November 17, 2025 AT 21:11Sarah Frey
November 18, 2025 AT 02:16Katelyn Sykes
November 18, 2025 AT 06:14Gabe Solack
November 19, 2025 AT 01:14Yash Nair
November 20, 2025 AT 23:30Bailey Sheppard
November 21, 2025 AT 14:24Girish Pai
November 22, 2025 AT 02:51Kristi Joy
November 23, 2025 AT 22:58