
Key Takeaways
- High blood pressure can accelerate bone loss and raise fracture risk.
- Inflammation, calcium loss, and hormone changes are the main culprits.
- Some antihypertensive drugs protect bones while others may worsen loss.
- Good nutrition, weight‑bearing exercise, and regular bone density tests can offset the damage.
- Talk to your doctor about blood‑pressure meds that fit your bone‑health profile.
Understanding the link between hypertension bone health helps you take proactive steps before damage sets in.
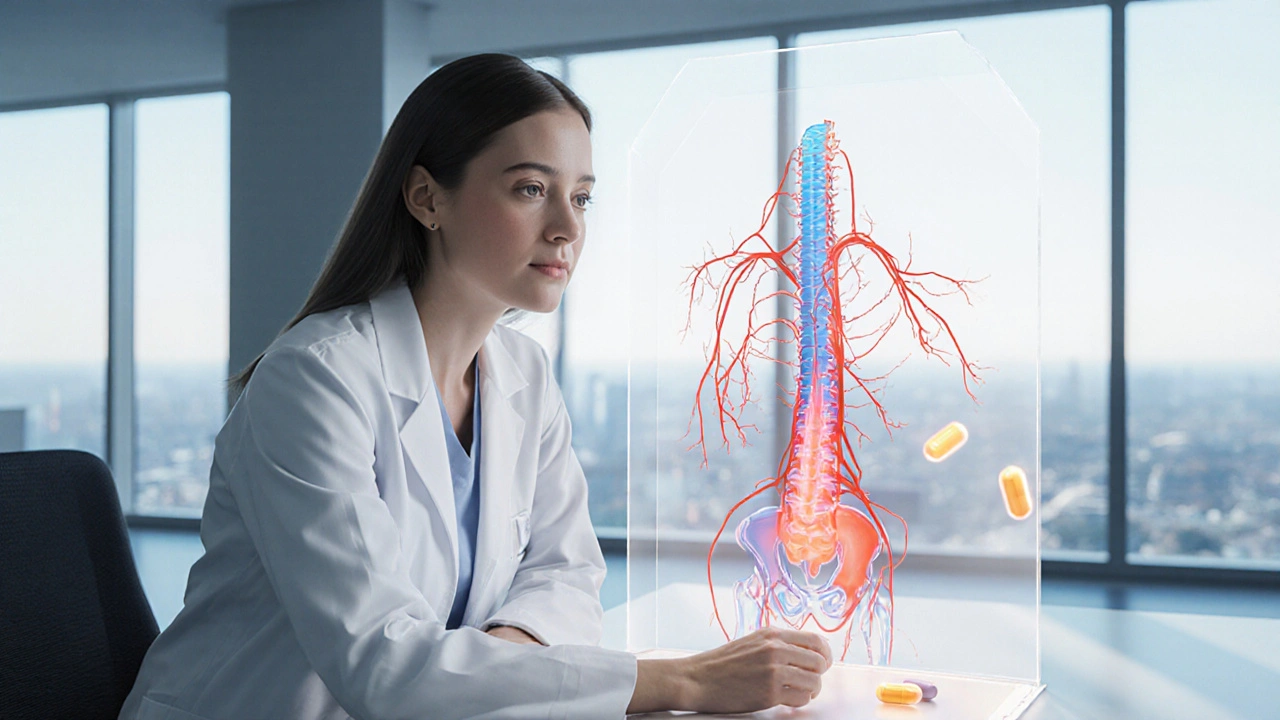
What Is Hypertension?
When we talk about Hypertension is a chronic condition where the force of blood against artery walls stays consistently high, we’re dealing with a silent driver of many health problems. The usual cutoff is 130/80mmHg or higher, according to the latest guidelines. Over time, that pressure strains the vascular system, sparks inflammation, and even tweaks the way the kidneys handle calcium and phosphate.
Bone Health 101
Healthy bones aren’t just rigid sticks; they’re living tissue that constantly rebuilds itself in a process called remodeling. Bone density measures the amount of mineral content packed into a cubic centimeter of bone is the gold‑standard metric doctors use to gauge strength. When density drops below a certain point, we call it osteoporosis a disease characterized by porous, fragile bones prone to fractures.
Why High Blood Pressure Hurts Your Bones
Three main pathways link hypertension to bone loss.
- Inflammatory cascade. Elevated pressure boosts circulating cytokines like interleukin‑6. Those molecules speed up osteoclast activity-the cells that chew away bone-while dampening osteoblasts, the builders.
- Calcium leakage. The kidneys try to flush out excess sodium, and calcium often tags along. Over time, calcium the primary mineral that gives bone its hardness excretion climbs, leaving the skeleton under‑supplied.
- Renin‑angiotensin system (RAS) interference. Renin‑angiotensin system a hormonal loop that regulates blood pressure also shows up in bone cells. Angiotensin II binds to receptors on osteoclasts, nudging them to work harder. Block that signal and you may see a modest bone‑preserving effect.
Parathyroid hormone a hormone that controls calcium levels by increasing bone resorption when blood calcium is low can also climb in people with uncontrolled hypertension, adding another route for calcium loss.
Medications: Friend or Foe?
Not all blood‑pressure pills act the same on bones.
- ACE inhibitors and ARBs. These drugs dial down the RAS pathway. Studies from 2023‑24 suggest they can modestly raise bone‑density scores, especially in post‑menopausal women.
- Beta‑blockers. The evidence is mixed; some data shows neutral impact, while others hint at a slight protective edge by lowering sympathetic nervous activity.
- Thiazide diuretics. They actually reduce calcium loss in urine, making them a top pick for patients worried about osteoporosis.
- Loop diuretics (e.g., furosemide). The opposite effect-more calcium rushes out, potentially accelerating bone demineralization.
- Calcium‑channel blockers. Generally neutral, though a few trials noted a small uptick in fracture risk, likely due to blood‑volume changes.
When your doctor prescribes a medication, ask whether it has bone‑safety data. A simple switch from a loop diuretic to a thiazide can make a noticeable difference over a decade.
Nutrition and Lifestyle Moves That Counteract the Damage
Even if you have high blood pressure, you can shield your skeleton with a few habit tweaks.
- Boost vitaminD. Vitamin D helps the gut absorb calcium and supports bone remodeling is essential. Aim for 800-1000IU daily, or more if you live far from the sun.
- Eat calcium‑rich foods. Dairy, fortified plant milks, sardines, and leafy greens supply the mineral you lose through the kidneys.
- Stay active. Weight‑bearing exercises-walking, jogging, resistance training-stimulate osteoblasts and improve balance, reducing fall risk.
- Limit sodium. Excess salt forces the kidneys to dump calcium. Keep daily intake below 2,300mg (about one teaspoon of table salt).
- Mind alcohol and caffeine. Heavy drinking and >3 cups of coffee a day can both erode bone density over time.
Screening: When and How to Check Your Bones
If you’re over 50, have a family history of fractures, or have been on hypertension meds for more than five years, talk to your doctor about a bone density test usually a DXA scan that measures mineral content in the hip and spine. The test is quick, non‑invasive, and often covered by health plans.
Key numbers to watch:
- T‑score≥‑1: normal
- T‑score between ‑1 and ‑2.5: low bone mass (osteopenia)
- T‑score≤‑2.5: osteoporosis
Even a borderline T‑score is a warning sign if you also have uncontrolled hypertension. Early intervention can keep you out of the ER.
Putting It All Together
Think of hypertension and bone health as two rooms in the same house. If the plumbing (blood pressure) leaks, the walls (bones) eventually get soggy. By fixing the leak-through medication choices, diet, and exercise-you protect both rooms at once.
Here’s a quick action plan:
- Get your blood pressure under the target range (ideally <130/80mmHg).
- Ask your prescriber whether your current antihypertensive has bone‑safety data; consider ACE inhibitors, ARBs, or thiazides if you’re at risk.
- Schedule a DXA scan if you’re 50+ or have additional risk factors.
- Load up on calcium+vitaminD and trim sodium.
- Add a 30‑minute walk or resistance routine most days of the week.
Follow these steps and you’ll give your skeleton a fighting chance, even if your heart has to work a little harder.

Frequently Asked Questions
Can hypertension cause fractures even if bone density looks normal?
Yes. High blood pressure can weaken bone micro‑architecture and increase fall risk, so fractures can happen before a DXA scan flags osteoporosis.
Which blood‑pressure meds are safest for someone with osteoporosis?
Thiazide diuretics, ACE inhibitors, and ARBs have the best bone‑protective track record. Loop diuretics should be avoided if possible.
How much vitaminD should I take if I have hypertension?
Most adults benefit from 800-1,000IU daily, but if you’re over 65 or have limited sun exposure, 2,000IU may be safer. Check with your doctor.
Is regular exercise enough to offset bone loss from high blood pressure?
Exercise helps a lot, but it works best when paired with good blood‑pressure control and adequate calcium/vitaminD intake.
Should I get a bone scan every year if I’m on antihypertensive medication?
Usually a scan every 2-3years is enough unless you have other risk factors. Your doctor can set a schedule based on your T‑score trends.



Jaspreet Kaur
September 29, 2025 AT 21:16Never thought about blood pressure and bones being connected but it makes sense now. We fix the leak before the house collapses.
Gina Banh
September 29, 2025 AT 23:50Dan Rua
September 30, 2025 AT 17:17Mqondisi Gumede
October 1, 2025 AT 11:54My grandpa had high BP and lived to 98 lifting cows and eating salted pork. Bone density tests are a scam invented by radiology departments to make money
Douglas Fisher
October 1, 2025 AT 12:19vikas kumar
October 1, 2025 AT 19:43Vanessa Carpenter
October 3, 2025 AT 10:23Bea Rose
October 5, 2025 AT 01:14Michael Collier
October 6, 2025 AT 00:46Deirdre Wilson
October 8, 2025 AT 00:41Damon Stangherlin
October 8, 2025 AT 23:30Ryan C
October 10, 2025 AT 11:10Albert Guasch
October 12, 2025 AT 03:09Ginger Henderson
October 13, 2025 AT 06:40Jesús Vásquez pino
October 14, 2025 AT 15:53