Every year, hundreds of thousands of people end up in the hospital because of drug interactions - and many of them could have been avoided with a simple change: timing. It’s not always about stopping a medication or swapping it out. Sometimes, all you need to do is take one pill two hours before another. Sounds easy? It’s not. But when done right, it can mean the difference between feeling better and ending up in the ER.
Why Timing Matters More Than You Think
Most people think drug interactions mean two medicines clash in the bloodstream and cause chaos. That happens sometimes - but a big chunk of dangerous interactions happen earlier: in your stomach and intestines. That’s where timing becomes your secret weapon. Take antibiotics like ciprofloxacin and antacids like Tums. If you take them together, the calcium and magnesium in the antacid bind to the antibiotic before it can be absorbed. Studies show this cuts the antibiotic’s effectiveness by up to 90%. But if you wait two hours after the antacid before taking the antibiotic? The drug gets absorbed just fine. No loss. No risk. Same goes for thyroid medicine like levothyroxine. If you take it with your morning coffee, cereal, or iron supplement, your body absorbs less than half of what it should. But if you take it on an empty stomach and wait four hours before anything else? You get nearly all the benefit. That’s why doctors tell you to take it first thing in the morning - and why so many people still get it wrong. These aren’t rare cases. About 20-30% of all documented drug interactions can be fixed just by changing when you take your pills. That’s one in every five to six interactions you might be told to worry about. And unlike swapping drugs or lowering doses, timing lets you keep all your medications - which matters a lot if you’re managing diabetes, heart disease, or depression.When Timing Won’t Help (And What to Do Instead)
Not every interaction can be solved with a clock. Some happen inside your liver, where enzymes break down drugs. If one medicine slows down how fast your body processes another, timing won’t fix it. The drugs are still interacting, no matter when you take them. For example, warfarin (a blood thinner) and metronidazole (an antibiotic) are a dangerous pair. Metronidazole blocks the enzyme that clears warfarin from your body. That means warfarin builds up, and your risk of serious bleeding skyrockets. You can’t fix this by spacing them out. You need to either stop one, switch to a different antibiotic, or get your blood tested more often to adjust the warfarin dose. Another example: grapefruit juice and statins. Grapefruit blocks an enzyme that breaks down certain cholesterol drugs. The result? Too much drug in your blood, which can damage your muscles. Even if you take the statin 12 hours after grapefruit, the enzyme is still blocked. The only fix is to avoid grapefruit entirely or switch to a statin that doesn’t interact - like pravastatin or rosuvastatin. So how do you know which is which? It’s simple: if the interaction is about absorption (one drug blocking another in your gut), timing helps. If it’s about metabolism (one drug changing how your liver handles another), timing doesn’t. Your pharmacist can tell you which is which - but you have to ask.Top 5 Medications That Need Strict Timing
Here are five common drugs that absolutely need spacing to work right - and how to get it right:- Levothyroxine (thyroid): Take on an empty stomach, first thing in the morning. Wait at least 4 hours before taking iron, calcium, or multivitamins. Even coffee can reduce absorption - wait 30-60 minutes after taking it.
- Alendronate (Fosamax): Take with a full glass of water, at least 30 minutes before eating or drinking anything else. Don’t lie down for 30 minutes after. If you take it with food or other meds, it won’t absorb properly - and your bones won’t get the benefit.
- Tetracycline or doxycycline (antibiotics): Avoid dairy, antacids, and iron supplements for at least 2-3 hours before and after. These bind to the antibiotic and make it useless.
- Fluoroquinolones (ciprofloxacin, levofloxacin): Same rule as tetracycline. No calcium, magnesium, aluminum, or iron within 2 hours. That includes antacids, multivitamins, and even some calcium-fortified orange juice.
- Proton pump inhibitors (PPIs) like omeprazole: These work best when taken 30-60 minutes before a meal. But if you’re also on iron supplements, space them at least 2 hours apart. PPIs reduce stomach acid, which iron needs to absorb properly.
What Works in Real Life - and What Doesn’t
Doctors and pharmacists have been using timing for years - but it’s not always easy to pull off. At UCSF Medical Center, pharmacist Jane Chen set up a simple protocol: for every patient on iron and a PPI, she added a note to their chart: “Take iron 2 hours after PPI.” Over 18 months, iron deficiency cases in older patients dropped by 32%. No new drugs. No extra cost. Just better timing. But not every story ends well. Nurse Mark Johnson in a New York hospital found that 40% of patients on 10+ medications couldn’t follow their timing schedules. They’d mix up which pill to take when. One man took his thyroid medicine with his blood pressure pill - and kept feeling tired. He didn’t realize the calcium in his BP med was blocking his thyroid drug. The solution? Tools. Digital pill reminders like Medisafe or MyTherapy cut adherence errors by 57% in a 2021 study. These apps let you set custom alerts for each pill - “Take levothyroxine now,” then “Wait 4 hours,” then “Take iron.” They even sync with family members or caregivers. Pill organizers with separate compartments for morning, afternoon, and evening help too. One study found they reduced timing mistakes by 43%. But only if the patient actually uses them right. A 77-year-old woman in Auckland told her doctor she was using her organizer - but she’d just dump all her pills in the morning slot. Timing didn’t matter to her. She just wanted to get it over with.How to Get Started - Step by Step
If you’re on five or more medications, you’re at higher risk. Here’s how to fix it:- Make a full list. Write down every pill, supplement, and over-the-counter drug you take - including vitamins, herbal teas, and antacids. Don’t leave anything out.
- Check for timing risks. Use a trusted source like Lexicomp or Micromedex (ask your pharmacist to show you). Look for interactions labeled “absorption” or “GI binding.”
- Map out your day. Group your meds by when you take them. Can you take all your morning pills at once? Or do some need space? Plan around meals, sleep, and your routine.
- Use reminders. Set alarms on your phone. Or use a pill app. Write a simple note on your pill bottle: “Wait 2 hours after Tums.”
- Review every 3 months. Your meds change. So should your schedule. Ask your pharmacist to check your timing plan every time you refill.

What to Do If You’re Confused
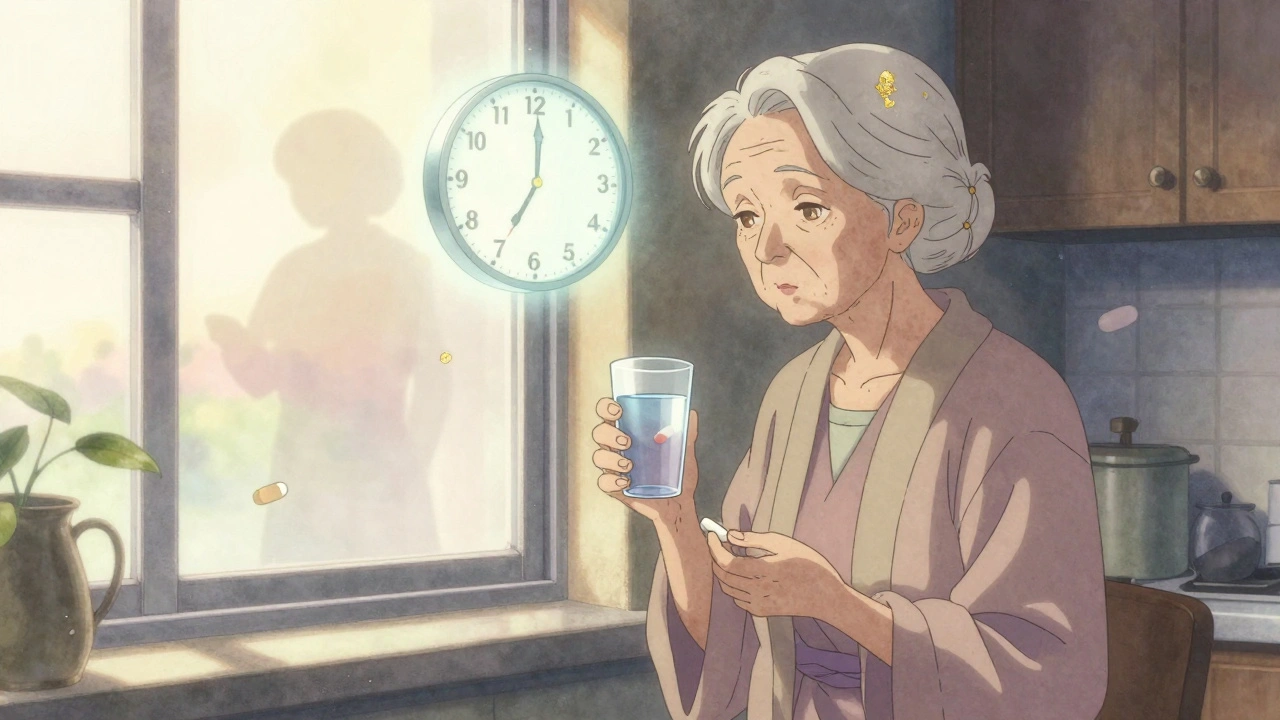
You’re not alone. Two out of three people over 65 say they’re confused about when to take their meds. That’s not your fault - it’s the system’s. If your doctor just says “Take this twice a day,” ask: “Is there anything I shouldn’t take with it? Do I need to wait?” If they don’t know, ask your pharmacist. They’re trained for this. Don’t guess. Don’t skip doses to “fix” timing. If you’re unsure, call your pharmacy. Most have free medication reviews. Take your bottles in. Let them walk you through it. And if you’re helping an older parent or relative? Don’t assume they remember. Sit with them. Show them the app. Put sticky notes on their pillbox. Make it simple.The Bigger Picture - Why This Is Getting More Important
More people are on more meds than ever. In the U.S., nearly half of adults over 65 take five or more drugs. That’s a recipe for timing disasters. Hospitals are catching on. Eighty-two percent now have computer systems that warn doctors when a new prescription might clash with an existing one - and suggest a time gap. But community pharmacies? Only 37% do this. That means you’re often the last line of defense. The FDA now requires drug labels to include timing advice for 17 high-risk pairs - like clarithromycin and colchicine. That’s progress. But labels are hard to read. You still need someone to explain them. And the cost? Not taking timing seriously leads to 115,000-178,000 preventable hospitalizations a year in the U.S. That’s billions in extra care. But for you? It’s not about money. It’s about staying out of the hospital, feeling well, and keeping your life normal.Final Thought: Timing Isn’t Optional - It’s Part of the Dose
A pill isn’t just a pill. Its effect depends on when you take it, what else is in your stomach, and how your body handles it. For some drugs, timing isn’t a suggestion - it’s part of the dose. If you’re on multiple medications, don’t just take them. Plan them. Talk about them. Use tools. Ask questions. You’re not being difficult - you’re being smart. Your health isn’t about taking pills. It’s about taking them right. And sometimes, that means waiting.Can I take my vitamins with my other medications?
It depends. Many vitamins - especially those with calcium, iron, magnesium, or zinc - can block absorption of antibiotics, thyroid meds, and bisphosphonates. Always check the label or ask your pharmacist. If you take a multivitamin, space it at least 2-4 hours away from your most sensitive meds. Some people take their vitamins at lunch or dinner to avoid conflicts with morning pills.
What if I forget to wait the recommended time?
Don’t panic. If you took two interacting meds together by accident, skip the next dose of the affected drug only if your doctor or pharmacist says to. For example, if you took ciprofloxacin with an antacid, don’t double up later - just wait until your next scheduled dose. Missing one dose won’t ruin your treatment, but doing it often will. Use reminders to avoid repeats.
Are natural supplements safe to take with prescription drugs?
No, not necessarily. St. John’s wort can reduce the effect of antidepressants, birth control, and blood thinners. Garlic and ginkgo can increase bleeding risk with warfarin. Even magnesium in supplements can interfere with antibiotics. Treat supplements like drugs - check for interactions. Many people assume “natural” means safe, but that’s not true.
Do I need to time my medications if I take them once a day?
Yes, if you’re taking more than one medication. Even once-a-day pills can interact. For example, if you take levothyroxine in the morning and a calcium supplement at night, you’re fine. But if you take both at the same time - even if it’s just once a day - the calcium will block absorption. Timing isn’t about frequency. It’s about what’s in your body at the same time.
Can my pharmacist help me set up a timing schedule?
Absolutely. Most pharmacies offer free medication reviews. Bring all your bottles - including supplements and OTC meds. Ask them to check for timing conflicts and help you build a simple daily plan. Many will even print out a color-coded chart or set up alerts in their app. Don’t wait until you feel sick - get it checked now.
Is it safe to use a pill organizer for timed medications?
Yes - but only if you use it correctly. A multi-compartment organizer helps if you can fill it with the right timing in mind. For example, if you need to wait 4 hours between thyroid and iron, don’t put both in the same day slot. Use separate organizers for morning and evening, or label compartments clearly. If you’re unsure, ask your pharmacist to help you fill it properly.





Rashmin Patel
December 3, 2025 AT 15:07Okay, I’ve been taking my levothyroxine with my morning coffee for years because my doctor said ‘take it on an empty stomach’ - I thought that meant no breakfast, not no caffeine. 🤦♀️ Now I’m switching to water only and waiting 45 minutes. If this doesn’t fix my fatigue, I’m suing my endocrinologist for not saying ‘coffee is a silent killer for thyroxine.’
Cindy Lopez
December 5, 2025 AT 09:22‘Wait two hours after antacids’ - this advice is technically correct but practically useless for people who take Tums three times a day because their stomach is always on fire. You can’t live like a monk just to make your cipro work. The real solution is prescribing alternatives that don’t suck.
Ignacio Pacheco
December 7, 2025 AT 00:33So let me get this straight - you’re telling me the reason I’ve been feeling like a zombie for six months is because I took my iron with my PPI? Not my depression meds, not my sleep issues, not my ‘aging’ - just timing? And you expect me to believe this isn’t just pharma pushing pills to sell apps?
James Kerr
December 8, 2025 AT 22:55Biggest win for me? Using Medisafe. I used to mix up my thyroid and calcium pills. Now my phone yells at me like a drill sergeant: ‘THYROID NOW. WAIT 4 HOURS. DO NOT IGNORE.’ I’m alive. And I didn’t even have to change my life. Just my phone settings. 🙌
Kidar Saleh
December 10, 2025 AT 18:04I work in a London pharmacy. Every Tuesday, Mrs. Henderson comes in with a plastic bag full of 17 different bottles. She doesn’t know what half of them are for. We sit down. We make a color-coded chart. She cries. We cry. Next week, she comes back smiling. Timing isn’t science - it’s dignity. And it’s free.
shalini vaishnav
December 10, 2025 AT 21:08Of course Americans need apps to remember when to take pills. In India, we’ve been taking 8+ medicines daily since the 1980s. We use our mothers’ voices as alarms. We don’t need notifications. We have discipline. This post is just another Western overcomplication of a simple concept: take your medicine. Period.
Jim Schultz
December 11, 2025 AT 22:45Let’s be honest - this entire article reads like a pharmaceutical marketing pamphlet disguised as medical advice. ‘Use our app!’ ‘Ask your pharmacist!’ ‘Don’t forget to wait!’ Where’s the data on actual mortality reduction? Where’s the peer-reviewed study proving timing reduces ER visits by more than 2%? This feels like fearmongering wrapped in bullet points.
Kara Bysterbusch
December 12, 2025 AT 09:06As someone who manages five chronic conditions and has spent years in medical libraries, I can confirm: timing is the most under-taught, under-resourced, and under-appreciated pillar of pharmacotherapy. The FDA’s 17 high-risk pairs? They’re a start - but there are over 300 documented absorption-based interactions. Medical schools should require a semester on this. Not a footnote in a pharmacology lecture. We are failing patients by treating medication timing as an afterthought - not a core clinical skill.
Rashi Taliyan
December 12, 2025 AT 18:45My mother took her levothyroxine with her calcium supplement for 12 years. She was always tired. Always cold. We thought it was ‘just old age.’ Then her pharmacist pointed out the timing issue. We changed it. Within three weeks, she started gardening again. No new drugs. Just space. I’ll never forget how she said, ‘I didn’t know I was still alive until I started taking my pills right.’
Albert Essel
December 12, 2025 AT 22:44One sentence: If you take a pill with grapefruit juice, stop. Now. It doesn’t matter if it’s 6 AM or 6 PM. The enzyme inhibition lasts 72 hours. This isn’t a myth. It’s biochemistry. And yes, your ‘natural’ orange juice with added pulp is just as dangerous. Don’t argue. Just stop.
sagar bhute
December 14, 2025 AT 13:33This is why medicine is broken. You spend 15 minutes with a doctor who prescribes you 12 pills, then you’re left to Google interactions like a detective. No one explains this stuff. No one cares. You’re supposed to be grateful for the pills, not the schedule. And if you die from a timing error? Well, that’s just bad luck.
vinoth kumar
December 15, 2025 AT 09:33I used to take my antibiotics with yogurt because I heard probiotics help. Turns out, the calcium in yogurt killed the cipro. I ended up with a kidney infection. Now I take my probiotics at bedtime, 4 hours after my last pill. Simple. Free. Life-changing. Thanks for the reminder - I almost forgot to share this with my uncle.
Vincent Soldja
December 15, 2025 AT 13:16Timing matters. But so does compliance. Most patients can’t follow these schedules. The real solution is single-pill combinations, extended-release formulations, and better drug design - not more reminders.
Chloe Madison
December 16, 2025 AT 05:50You’re not lazy for forgetting. You’re not stupid for mixing pills. You’re just human. And this system? It’s designed for perfect people who have no jobs, no kids, no anxiety, and no memory. But here’s the good news: you don’t need to be perfect. Just consistent. One change. One app. One conversation with your pharmacist. That’s all it takes to go from ‘I feel awful’ to ‘I feel like me again.’ You got this.
Gene Linetsky
December 16, 2025 AT 21:21Wait… so the government knows about this but doesn’t force pharmacies to print timing warnings on every bottle? And the FDA only mandates it for 17 pairs? That’s not oversight - that’s corruption. Big Pharma doesn’t want you to know timing can replace expensive drugs. They want you buying new prescriptions every month. This isn’t medicine. It’s a money scheme disguised as science.