
CYP2C19 Drug Interaction Calculator
This calculator estimates how much omeprazole or other PPIs reduce clopidogrel effectiveness based on your medication type, dose, and genetic factors. Use it to discuss safer alternatives with your doctor.
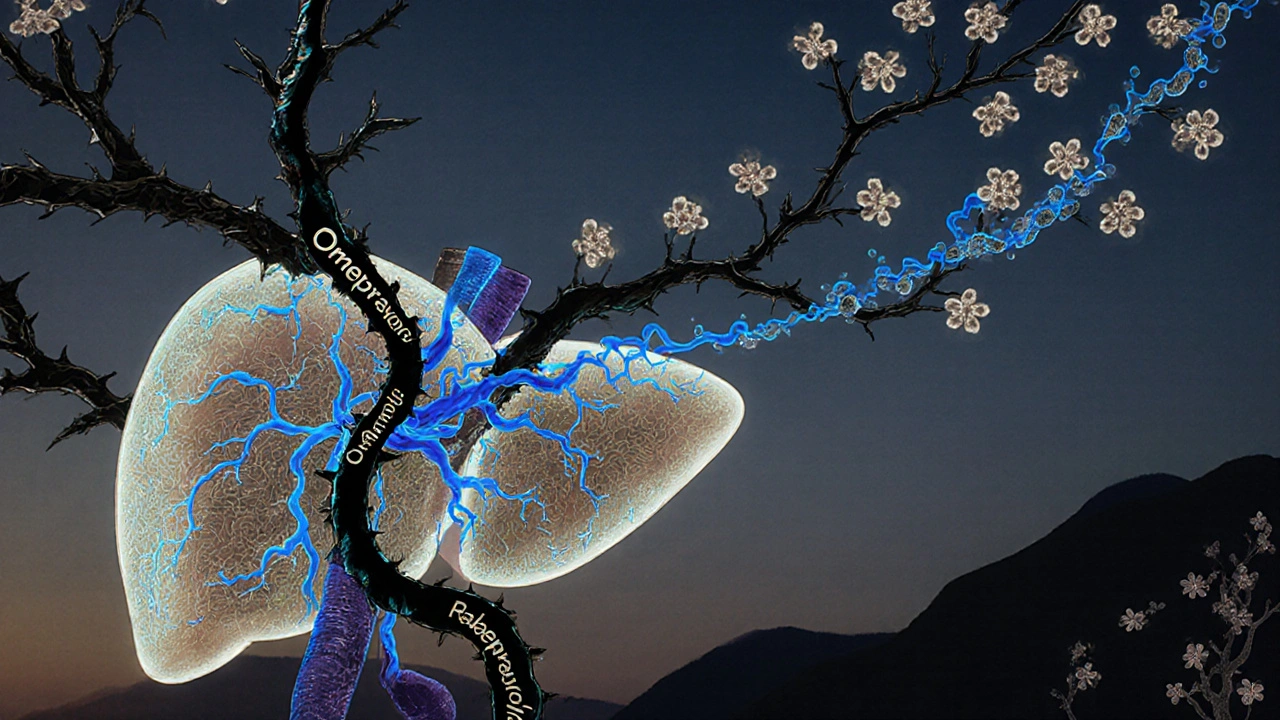
If you're taking clopidogrel to prevent heart attacks or strokes, and your doctor also prescribed omeprazole for acid reflux or ulcers, you might be unaware of a hidden conflict between these two common drugs. It’s not about side effects like nausea or dizziness-it’s about whether clopidogrel even works at all. The problem lies in your liver, specifically in an enzyme called CYP2C19. This enzyme is the key that unlocks clopidogrel’s power. And omeprazole? It’s the lockpick that jams the keyhole.
How Clopidogrel Actually Works (It’s Not What You Think)
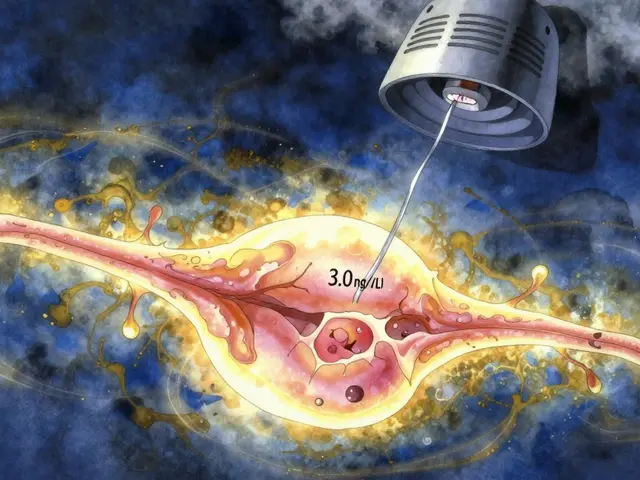
Clopidogrel doesn’t do anything on its own. It’s a prodrug-meaning your body has to turn it into something active before it can stop blood clots. That transformation happens mostly in the liver, and CYP2C19 is the main enzyme responsible. Without it, clopidogrel stays useless. Think of it like a key that needs to be cut before it can open a door. Omeprazole doesn’t just sit there; it actively blocks CYP2C19 from doing its job.Studies show that when you take omeprazole with clopidogrel, the amount of active clopidogrel in your blood drops by up to 49%. That’s not a small dip-it’s a major drop. The FDA flagged this back in 2009 after research from Brandt and Sibbing showed that omeprazole 80mg reduced clopidogrel’s active metabolite by 45%. Even the standard 20mg dose cuts effectiveness by about 32%. And here’s the kicker: the higher the dose of omeprazole, the worse it gets.
Why Omeprazole Is the Worst Offender
Not all acid reducers are created equal when it comes to CYP2C19. Omeprazole is the strongest inhibitor among proton pump inhibitors (PPIs). Its binding affinity to CYP2C19 is so high that it outcompetes clopidogrel for the enzyme’s attention. In lab tests, omeprazole has an IC₅₀ value of 2-4 μM-meaning it shuts down the enzyme at very low concentrations. Compare that to pantoprazole (10-15 μM) or rabeprazole (15-20 μM), which barely make a dent.Esomeprazole, the more expensive version of omeprazole, isn’t any better. It’s just the purified S-isomer of omeprazole and behaves almost identically. Lansoprazole is slightly less problematic, but at high doses (60mg), it still cuts clopidogrel’s peak levels by 18%. Rabeprazole? It reduces peak levels by 28% in normal metabolizers, but doesn’t affect overall exposure-so it’s a gray area. But omeprazole? It hits both peak levels and total exposure hard.
The Genetic Factor: Why Some People Are at Higher Risk
Not everyone reacts the same way. About 30% of East Asians and 20-25% of Caucasians carry a genetic variant called CYP2C19*2 or *3. These are loss-of-function alleles. In simple terms, their bodies already make less of the enzyme needed to activate clopidogrel. Add omeprazole into the mix, and their clopidogrel effectiveness can plummet by over 50%.A Korean study found that in people with normal CYP2C19 function, omeprazole cut clopidogrel’s effect by 32%. But in those with intermediate metabolism (one bad gene copy), the drop jumped to 54%. That’s not just a warning-it’s a red flag. The Clinical Pharmacogenetics Implementation Consortium (CPIC) recommends switching to prasugrel or ticagrelor for these patients, especially if they need a PPI. These newer antiplatelets don’t rely on CYP2C19, so they’re unaffected by omeprazole.
What the Studies Really Say About Heart Attacks and Strokes
Here’s where things get messy. On paper, omeprazole clearly reduces clopidogrel’s activity. But does that translate to more heart attacks or strokes? The data says: maybe, maybe not.The COGENT trial in 2010, which randomly assigned over 3,700 patients to take omeprazole or placebo with clopidogrel, found no increase in cardiovascular events. That study used only 10mg of omeprazole-a low dose. Meanwhile, a massive meta-analysis of 271,551 patients showed a 27% higher risk of heart events with any PPI use, and a 33% higher risk specifically with omeprazole. The FAST-MI Registry, tracking over 2,700 patients, found no link. So which one do you trust?
The truth is, the clinical impact depends on your individual risk. If you’ve had a recent stent, a heart attack, or are high-risk for clotting, even a small drop in clopidogrel’s effect could be dangerous. If you’re stable, on low-dose clopidogrel, and have no history of clots, the risk may be minimal. But you can’t assume safety. That’s why guidelines don’t take chances.
What Doctors Actually Recommend Now
Major cardiology groups-American Heart Association, European Society of Cardiology, American College of Cardiology-all agree: avoid omeprazole and esomeprazole with clopidogrel. That’s not a suggestion. It’s a recommendation backed by pharmacokinetic data and regulatory warnings.If you need a PPI for stomach protection, pantoprazole is the go-to alternative. At 40mg daily, it barely affects clopidogrel. Rabeprazole is a second choice. And if you’re looking for something even safer, ilaprazole-a newer PPI not yet widely available in the U.S.-shows almost no inhibition in recent studies. But it’s not on the market everywhere yet.
Timing doesn’t help. Some people think taking clopidogrel in the morning and omeprazole at night will solve the problem. It won’t. CYP2C19 inhibition is ongoing. The enzyme doesn’t reset overnight. A 2013 study confirmed that separating doses by 12 hours made zero difference in clopidogrel’s antiplatelet effect.

What to Do If You’re Currently Taking Both
If you’re on clopidogrel and omeprazole right now, don’t stop either one without talking to your doctor. But here’s what to ask for:- Can we switch from omeprazole to pantoprazole?
- Would I be a candidate for ticagrelor or prasugrel instead of clopidogrel?
- Should I get tested for CYP2C19 genotype? (It’s becoming more common in cardiology clinics.)
- Is famotidine (an H2 blocker) an option? It doesn’t interfere with CYP2C19 and can still protect your stomach.
Since the FDA warning in 2009, prescriptions for omeprazole with clopidogrel dropped by 65% in the U.S. Meanwhile, pantoprazole use rose by 42%. That shift didn’t happen by accident. It happened because doctors started listening to the science.
The Bottom Line
Omeprazole isn’t just another pill. When paired with clopidogrel, it’s a silent saboteur. It doesn’t cause side effects-it causes failure. And the failure isn’t theoretical. It’s measurable in blood tests, in platelet activity, and in real-world outcomes for high-risk patients.You don’t need to avoid all PPIs. You just need to avoid the ones that block CYP2C19. Omeprazole and esomeprazole are the worst. Pantoprazole and rabeprazole are safer. Ticagrelor and prasugrel are better alternatives if you need stronger, more reliable antiplatelet therapy.
Genetics matter. Your dose matters. Your medical history matters. But most of all, your conversation with your doctor matters. Don’t assume your meds are safe just because they’re commonly prescribed. Ask the question: Is this combination really working for me-or is it quietly letting my blood clot?




jalyssa chea
November 17, 2025 AT 05:27OMG i was on both and had a mini stroke last year no joke
Rob Goldstein
November 18, 2025 AT 11:33Really glad someone laid this out so clearly. CYP2C19 is such a sneaky one-most docs don’t even bring it up unless you’re high risk. I’ve seen patients on clopidogrel for years, then get omeprazole for heartburn, and boom-platelet reactivity spikes. The lab tests don’t lie. Switching to pantoprazole? Game changer. And if you’re Asian or have a family history of clotting, get genotyped. It’s cheap now and saves lives.
Peter Stephen .O
November 18, 2025 AT 18:33Bro this is wild. Omeprazole is basically the silent killer of your heart meds. Like imagine your body has a key factory and omeprazole shows up with a sledgehammer and smashes all the key-cutting machines. And you’re out there thinking you’re protected from clots but your blood’s just doing the cha-cha. I’ve been on ticagrelor since my stent and honestly? It’s like night and day. No more worrying about my Tums. Also-famotidine? That’s the OG chill uncle of acid reducers. Doesn’t care about your liver’s schedule. Try it. Your CYP2C19 will thank you.
vinod mali
November 19, 2025 AT 14:21My uncle in India was on both and had a heart attack. Doctor said it was coincidence. But now I check all his meds. This post saved me from making same mistake. Thank you.
Julie Roe
November 19, 2025 AT 20:59I’m a nurse in cardiology and I’ve seen this play out too many times. A patient comes in with chest pain, they’re on clopidogrel, they’re also on omeprazole for ‘just a little heartburn,’ and their platelet function test shows near-zero inhibition. We had one guy who had a second stent within 4 months because he didn’t know the two drugs were fighting. When we switched him to pantoprazole, his platelet reactivity normalized in 10 days. It’s not even close to a debate anymore. The science is rock solid. What’s frustrating is how many primary care docs still prescribe omeprazole like it’s harmless. It’s not a ‘maybe’-it’s a ‘don’t.’ And if you’re on it? Talk to your cardiologist. Don’t wait for a crisis. Your liver is doing the math right now-and it’s not adding up.
Also, if you’re over 65, on aspirin, and on a PPI? You’re already at higher GI risk. So yes, you need stomach protection. But you don’t need omeprazole. Pantoprazole is fine. Rabeprazole is fine. Even H2 blockers like famotidine work. Just don’t let convenience kill you. And yes, the FDA warning was in 2009. We’ve had 15 years. Why are we still having this conversation?
And for the love of all that’s holy, don’t think splitting doses helps. I’ve had patients try taking clopidogrel at 7am and omeprazole at 11pm. It’s like putting a bandaid on a broken leg. The enzyme doesn’t take a break. It’s blocked all day. Every. Single. Day.
And if you’re thinking ‘but my doctor said it’s fine’-ask them if they’ve read the CPIC guidelines. If they haven’t, maybe it’s time to find one who has.
This isn’t fearmongering. This is pharmacology. And your life is worth knowing the details.
Kathy Grant
November 19, 2025 AT 21:44It’s funny how we trust pills like they’re magic spells. We swallow them without asking who’s in the room with them. Omeprazole doesn’t just ‘help your stomach’-it’s a silent negotiator in your liver, quietly trading away your heart’s protection for a little less acid. And we don’t even notice until it’s too late. I think we’ve lost the art of asking ‘what else is this changing?’ We just want the symptom gone. But biology doesn’t work in silos. It’s all connected. That little pill? It’s not just treating reflux. It’s rewiring your blood’s ability to stay fluid. And that’s… heavy. Maybe we need to start seeing meds not as fixes, but as conversations-with our bodies, with enzymes, with genes. And sometimes, the conversation is a fight. And you need to know who’s winning.
Gary Lam
November 21, 2025 AT 00:14So omeprazole is the villain and pantoprazole is the hero? Man, I thought I was just taking my daily ‘heartburn insurance.’ Turns out I was paying for my own clotting risk. Thanks for the reality check, doc. I’m switching to pantoprazole tomorrow. Also, I’m calling my doctor and asking if I can get ticagrelor so I can stop caring about all this. I’m tired of being a pharmacology lab rat.
Jennie Zhu
November 21, 2025 AT 21:01It is imperative to recognize that the pharmacokinetic interaction between omeprazole and clopidogrel is mediated through competitive inhibition of the cytochrome P450 2C19 isoenzyme, resulting in a significant reduction in the formation of the active thiol metabolite of clopidogrel, thereby diminishing its antiplatelet efficacy. Clinical evidence from multiple prospective cohort studies and meta-analyses supports a statistically significant association between concomitant use and increased incidence of major adverse cardiovascular events, particularly in patients with loss-of-function alleles. The American College of Cardiology and European Society of Cardiology guidelines strongly recommend avoidance of omeprazole and esomeprazole in this context, with pantoprazole or rabeprazole as preferred alternatives. Pharmacogenetic testing for CYP2C19 polymorphisms is increasingly indicated in high-risk populations.
Robert Merril
November 23, 2025 AT 02:05Wait so if i take omeprazole at night and clopidogrel in morning it works right? My doctor said so and i dont wanna change. Also i think the FDA is just scared of big pharma. Also i saw a video on tiktok that said all PPIs are poison anyway so maybe im better off with apple cider vinegar? 🤔
Andrew Cairney
November 24, 2025 AT 02:58THEY KNOW. THEY ALL KNOW. Omeprazole was designed to make you dependent. The FDA didn’t warn you because they’re scared. The real reason they want you off omeprazole? It’s not about clopidogrel. It’s because they’re pushing ticagrelor-$400 a month-and they want you hooked. Look at the stats: pantoprazole sales went up 42%? That’s not science-that’s corporate sabotage. And they’re using ‘CYP2C19’ like a cult chant to scare you into buying expensive drugs. I checked my own bloodwork. My platelets are fine. I’m not falling for it. This is all a scam to sell you more pills. Ask yourself: who profits? Big Pharma. Always.
Also I think the ‘genetic testing’ thing is just to make you feel broken. You’re not defective. You’re being manipulated. I’m going to start taking garlic and lemon water. It’s cheaper. And it doesn’t have a CYP code.
Noel Molina Mattinez
November 26, 2025 AT 02:28My doc switched me to pantoprazole after I asked and I haven't had heartburn since. Also my blood test showed better platelet response. So yeah. Do it. Just switch. No big deal.