
Theophylline Clearance Estimator
How theophylline interactions work
Theophylline has a narrow therapeutic window (10-20 mcg/mL). Many common medications inhibit the CYP1A2 enzyme that clears it from your body. This tool estimates how much your clearance might decrease and your potential toxicity risk.
Estimated Clearance Change
100%Your estimated clearance may decrease by 0% based on selected medications.
When you take theophylline for asthma or COPD, even a small change in your body’s ability to process it can turn a safe dose into a life-threatening one. The drug has a razor-thin margin between helping you breathe and pushing you into toxicity. And the biggest danger? It’s not always the dose you’re taking-it’s what else you’re taking.
Why Theophylline Is So Fragile
Theophylline isn’t like most asthma meds. While inhalers target your airways directly, theophylline works systemically. About 90% of it gets broken down in your liver by an enzyme called CYP1A2. That’s the same enzyme that processes caffeine, nicotine, and dozens of other common drugs. The problem? This enzyme doesn’t work at a steady rate. At therapeutic levels, the system gets overwhelmed. A tiny increase in the amount of theophylline-or a small drop in how fast it’s cleared-can cause levels to spike out of control.Normal clearance in a healthy adult is about 3 liters per hour. But that number can swing wildly. Smokers clear it faster-up to 1.2 mL/kg/h. Elderly patients with heart failure? As low as 0.35 mL/kg/h. And if you start a new medication that blocks CYP1A2? Your clearance can plummet by 40% or more. That’s not a 40% drop in effectiveness. That’s a 40% drop in how fast your body removes the drug. Result? Serum levels climb fast, and you’re at risk for seizures, irregular heartbeats, or even death.
Medications That Slow Down Theophylline Clearance
Not all drugs affect theophylline the same way. Some barely move the needle. Others? They’re dangerous.- Fluvoxamine (an antidepressant): Reduces clearance by 40-50%. This is one of the most dangerous combinations. The European Respiratory Society says to avoid it entirely. A patient on 300 mg of theophylline daily could see levels jump from 15 mcg/mL to over 25 mcg/mL within days-well into the toxic range.
- Cimetidine (for heartburn): Slows clearance by 25-30%. It’s old, cheap, and still used. But in a 2021 study of hospitalized patients, cimetidine was the top culprit in theophylline toxicity cases, involved in nearly 29% of incidents.
- Allopurinol (for gout): Lowers clearance by 20%. Many doctors don’t realize this interaction exists. A 600 mg daily dose of allopurinol can push theophylline levels into danger. Even lower doses (300 mg) can be risky if the patient is already near the top of the therapeutic range.
- Erythromycin and clarithromycin (antibiotics): Reduce clearance by 15-25%. These are common for respiratory infections, which is exactly when someone on theophylline might need them. That’s a double whammy: infection stresses the body, and the antibiotic slows drug clearance.
- Furosemide (water pill): Mixed evidence. Some studies show a 10-15% drop in clearance; others show no effect. But if a patient is already on the edge, even a small reduction can tip them over.
These aren’t rare cases. A 2023 survey of 412 pulmonologists found that nearly 8 out of 10 had seen a serious interaction in the past year. And in over 60% of theophylline toxicity cases in hospitals, the patient was taking at least one of these drugs.
What Happens When Levels Rise
The therapeutic window for theophylline is 10 to 20 mcg/mL. Anything above 20 is risky. Above 30? It’s a medical emergency.Early signs of toxicity are easy to miss: nausea, vomiting, headache, jitteriness. Patients often think it’s just the flu or stress. But if levels keep climbing, you get rapid heartbeat, tremors, seizures, or life-threatening arrhythmias. In 2022, the FDA reported over 1,800 adverse events linked to theophylline. More than 40% of those were due to drug interactions.
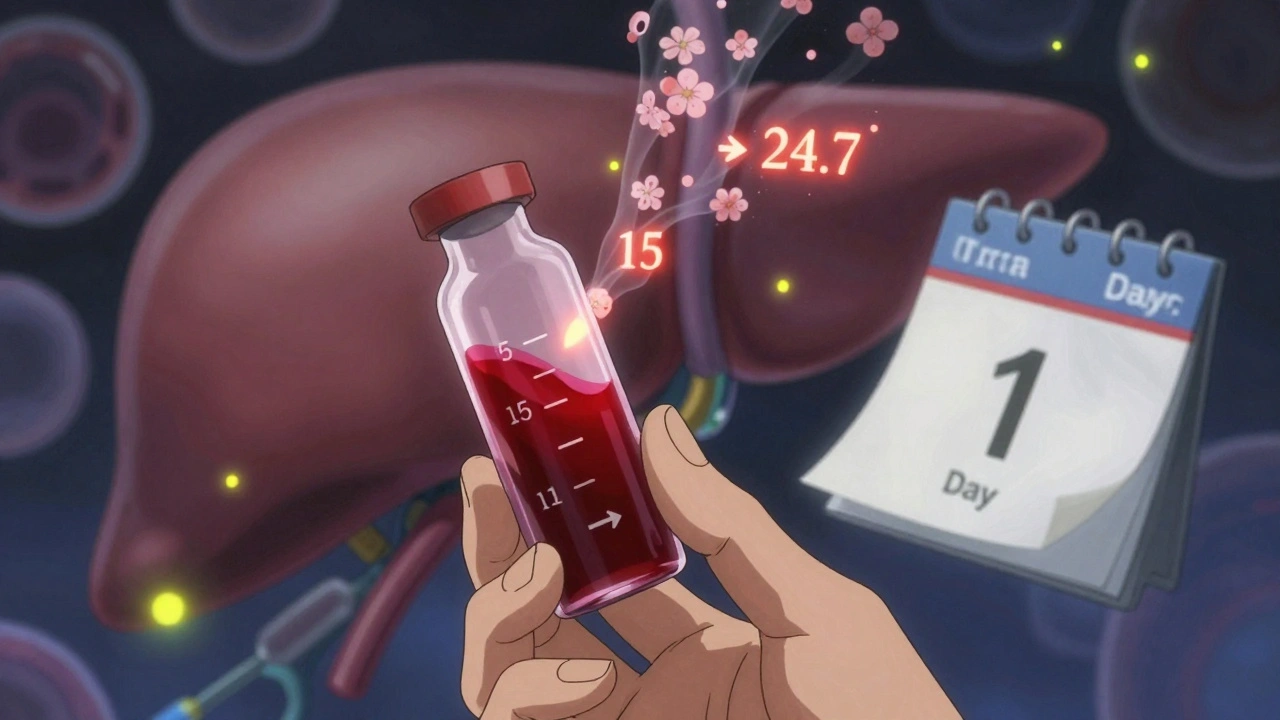
One real case from a community pharmacy in Ohio: A 72-year-old man with COPD had been on 200 mg of theophylline twice daily for years. His levels were steady at 15.2 mcg/mL. Then his doctor prescribed cimetidine for acid reflux. Three days later, he showed up at the ER with palpitations and vomiting. His theophylline level? 24.7 mcg/mL. He hadn’t changed his dose. The cimetidine did it.
What You Should Do
If you’re on theophylline, here’s what matters:- Know your meds. Make a list of every pill, supplement, and OTC drug you take. Include antacids, cold medicines, and sleep aids. Many contain hidden CYP1A2 inhibitors.
- Ask before starting anything new. Even if it’s just a short course of antibiotics or a new painkiller. Say: “I’m on theophylline. Is this safe?”
- Get your blood tested. The American Association for Clinical Chemistry recommends checking theophylline levels within 48 to 72 hours after starting or stopping any new medication. Don’t wait for symptoms.
- Don’t quit smoking cold turkey. Smoking induces CYP1A2. When you stop, your clearance drops by 30-50% within two weeks. If you’re on theophylline and quit smoking, your dose likely needs to be lowered. This interaction is often overlooked.
Some doctors still prescribe theophylline because it’s cheap and works. But they’re not always trained in its risks. A 2021 study found that only 37% of elderly patients on theophylline who were also taking interacting drugs had their doses adjusted. That’s a dangerous gap.
What’s Changing
Newer bronchodilators like long-acting beta agonists have replaced theophylline in most places. In the U.S., its use has dropped by 62% since 2000. But it’s still used in resource-limited areas, and for patients with severe nocturnal asthma who don’t respond to other treatments.There’s also new research into very low-dose theophylline (100-200 mg daily) for its anti-inflammatory effects in COPD. But these trials are strict: patients on CYP1A2 inhibitors are excluded. Why? Because the risk isn’t worth it.
Some hospitals are now using pharmacist-led monitoring programs. One at the University of Pittsburgh cut hospitalizations from theophylline toxicity by 37% in just one year. The key? Proactive checks, not waiting for emergencies.
The Bottom Line
Theophylline isn’t going away. But it’s a drug that demands respect. It’s not the kind of medication you can take casually. If you’re on it, you need to treat it like a precision tool-not a general-purpose pill.One extra pill, one new antibiotic, one change in smoking habits-these aren’t minor details. They’re potential triggers for a medical crisis. The best defense? Awareness. Communication. And blood tests.
If you’re on theophylline and your doctor prescribes something new, don’t assume it’s safe. Ask. Get tested. Don’t wait for symptoms. Your life depends on it.
Can I take ibuprofen with theophylline?
Yes, ibuprofen doesn’t significantly affect CYP1A2 and is generally safe with theophylline. But always check with your doctor or pharmacist, especially if you’re taking high doses or have kidney issues. Other NSAIDs like naproxen or diclofenac are also low-risk, but individual responses can vary.
How long does it take for theophylline levels to change after starting a new drug?
It can take 2 to 5 days for levels to reach a new steady state after starting or stopping a drug that affects CYP1A2. But dangerous spikes can occur within 48 hours. That’s why blood tests are recommended at 48-72 hours after starting a new medication.
Is theophylline still used today?
Yes, but much less than before. It’s mostly used in resource-limited settings or for patients with severe, refractory asthma or COPD who don’t respond to inhalers. Global use is highest in Asia and Africa, where newer drugs may be too expensive. In the U.S., it’s prescribed in only about 1.7% of COPD cases.
Can I drink coffee while taking theophylline?
Caffeine is metabolized by the same liver enzyme as theophylline. Drinking large amounts of coffee or energy drinks can compete for metabolism and slightly raise theophylline levels. If you’re a heavy coffee drinker, your doctor may need to adjust your dose. Moderate intake (1-2 cups a day) is usually fine, but monitor for jitteriness or palpitations.
What should I do if I miss a dose of theophylline?
Don’t double up. If you miss a dose, take it as soon as you remember-but only if it’s within a few hours of your scheduled time. If it’s close to your next dose, skip it. Theophylline has a narrow window, and overdosing can be dangerous. Always check with your provider before making changes.
Are there any over-the-counter supplements that interact with theophylline?
Yes. Some herbal products like St. John’s Wort can induce metabolism and lower theophylline levels, making it less effective. Others, like green tea extract or certain multivitamins with high doses of niacin, may inhibit CYP1A2. Always tell your doctor about supplements-many are not tested for drug interactions.




Rebecca Dong
December 9, 2025 AT 15:29Okay but what if the whole theophylline thing is just a Big Pharma scam to keep people hooked on blood tests? I mean, why do they even make this drug if it’s this dangerous? They know people will mix it with coffee and cimetidine-so why not just ban it and push inhalers? It’s all about the money. They profit off the panic. I’ve seen it before.
Stephanie Maillet
December 10, 2025 AT 07:44It’s fascinating how such a simple biochemical pathway-CYP1A2-can become a silent killer, isn’t it? The body’s metabolism is this delicate, elegant machine… and we, with our casual pill-popping habits, treat it like a vending machine. We don’t consider that every drug, every cup of coffee, every cigarette, is a tiny wrench tossed into the gears. Theophylline doesn’t ‘fail’-it’s the system that’s been quietly, tragically overloaded.
Raj Rsvpraj
December 12, 2025 AT 01:40Of course Americans are dying from this-because you all take 17 different pills and think ‘natural remedies’ are better than science. In India, we don’t have the luxury of mixing ibuprofen with antibiotics and then asking if it’s safe. We take what the doctor gives us, no questions, no coffee, no supplements. You think your ‘ask your doctor’ culture is smart? It’s just a recipe for disaster. Theophylline is for the disciplined-not the Instagram health gurus.
Frank Nouwens
December 12, 2025 AT 03:09This is one of those posts that makes you pause and re-read every medication you’ve ever taken. I’ve been on theophylline for years-never knew about the cimetidine risk. Thanks for laying it out so clearly. I’m going to call my pharmacist tomorrow and get my levels checked. Better safe than sorry, right?
Aileen Ferris
December 13, 2025 AT 09:15so like… if i quit smoking and im on theophylline… do i just like… die? lol jk but also not jk. my uncle did this and ended up in the er. they said he was lucky. he’s still alive but now he’s got a new med. i think i’m gonna stop smoking. for real this time.
Michelle Edwards
December 15, 2025 AT 01:15You’re not alone if this feels overwhelming. I’ve been on theophylline since I was 16, and I still get nervous every time I get a new prescription. But you’ve got this. Keep that list. Ask the questions. Get the blood work. You’re not being paranoid-you’re being smart. And that’s worth celebrating.
Neelam Kumari
December 16, 2025 AT 20:39Wow. So you’re telling me that people who drink coffee and take heartburn meds are basically playing Russian roulette with their heart? And they wonder why they’re tired all the time? No wonder the U.S. has so many ‘unexplained’ cardiac events. It’s not mystery illness-it’s just laziness and ignorance wrapped in a prescription bottle.
Queenie Chan
December 17, 2025 AT 16:19It’s like theophylline is the Mozart of drugs-brilliant, nuanced, and utterly unforgiving if you don’t treat it with reverence. One wrong note-a new antibiotic, a caffeine binge, a nicotine withdrawal-and the whole symphony turns into a scream. I love that this post doesn’t just list dangers-it paints the whole orchestra. The liver isn’t a trash can. It’s a conductor. And we’re the amateurs holding the baton.
Michaux Hyatt
December 18, 2025 AT 00:18Just wanted to add something practical: if you’re on theophylline and your doctor prescribes anything new, even a Z-pack, ask if they’ve checked the interaction. If they look confused? That’s your sign to ask for a pharmacist consult. Most hospitals have them for free-use them. I’ve seen too many patients get caught off-guard because the doctor ‘didn’t think it mattered.’ It always matters.
Jack Appleby
December 19, 2025 AT 11:28Let’s be honest-this post is basic pharmacology 101. If you’re a medical professional and you didn’t know about CYP1A2 interactions with theophylline, you shouldn’t be prescribing anything. The fact that 60% of toxicity cases involve these drugs isn’t a revelation-it’s a scandal. And the FDA’s 1,800 adverse events? That’s not a statistic. That’s 1,800 people who got failed by the system.
Kaitlynn nail
December 20, 2025 AT 00:01life hack: if you’re on theophylline, just stop taking everything. except theophylline. and maybe water. and maybe oxygen. that’s it. problem solved.
Sarah Clifford
December 21, 2025 AT 17:22so like… what if the real problem is that we’re all just too lazy to read the damn leaflet? i mean, i didn’t even know cimetidine was still a thing. who even uses that anymore? and why do people still take it with theophylline? like… are we all just on autopilot?
Regan Mears
December 23, 2025 AT 09:49One thing I’ve learned from working in ER: the people who survive theophylline toxicity are the ones who speak up. Not the ones who ‘assume it’s fine.’ Not the ones who ‘didn’t think it mattered.’ The ones who said, ‘I’ve been feeling off since I started this new pill.’ That’s the difference between a scary night in the ER and a funeral. Don’t wait for the tremors. Don’t wait for the seizure. Say something. Early.