
Blood Thinner Safety Calculator
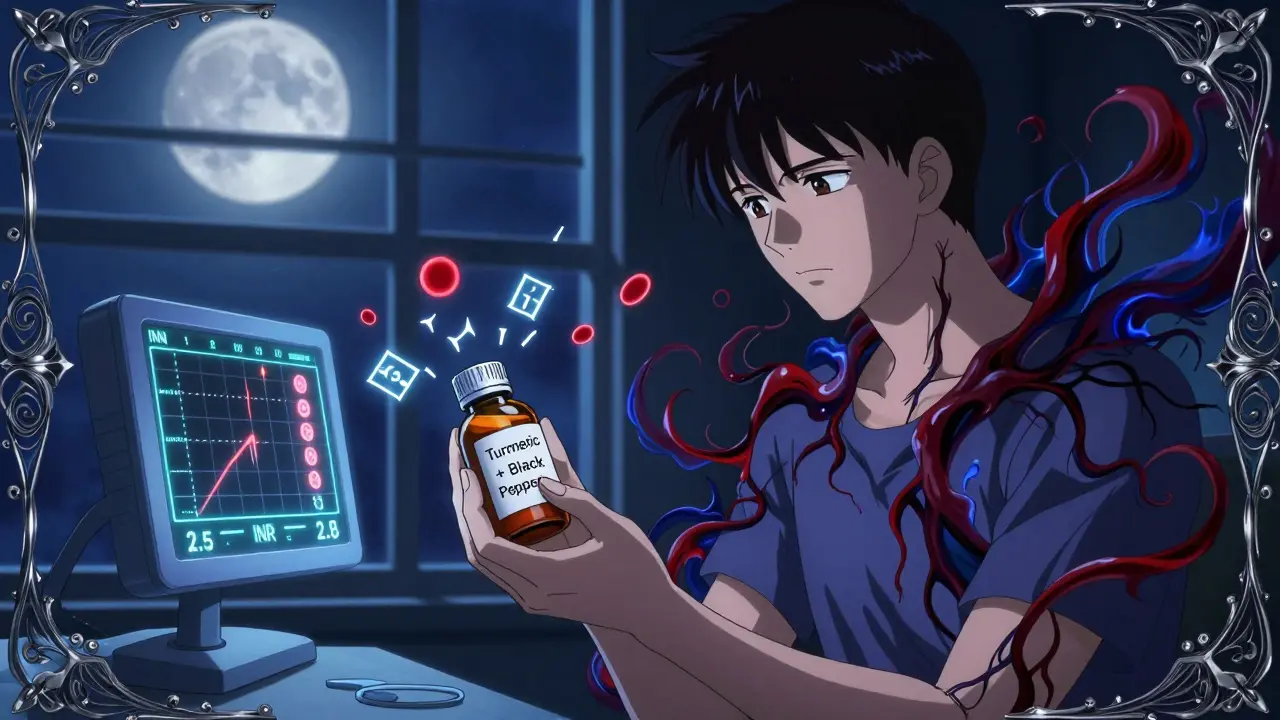
How Turmeric Affects Your Blood Thinner
This tool calculates your risk of dangerous bleeding when taking turmeric supplements with blood thinners. Based on the latest medical guidelines, we assess the interaction based on your specific medication.
Many people take turmeric supplements hoping to reduce inflammation, ease joint pain, or boost overall health. But if you're on a blood thinner, this common supplement could put you in serious danger. The problem isn't just turmeric-it's the turmeric and black pepper combo you'll find in nearly every bottle on the shelf. What’s marketed as "enhanced absorption" is actually a hidden risk that could lead to uncontrolled bleeding, liver damage, or even hospitalization.
Why Turmeric and Blood Thinners Don’t Mix
Turmeric contains curcumin, a compound that naturally thins the blood. It does this by slowing down platelet clumping and reducing substances that help blood clot. That sounds helpful-until you're already taking a prescription blood thinner like warfarin, apixaban, or clopidogrel. Then, turmeric doesn’t just add to the effect-it multiplies it.Doctors have seen real cases where patients with stable INR levels (a key test for blood thinning) suddenly had dangerous spikes after starting turmeric supplements. One documented case involved a man on warfarin whose INR jumped from 2.5 to 8.1 after taking a daily turmeric capsule for just three weeks. That’s not just elevated-it’s life-threatening. An INR above 4.5 significantly raises the risk of internal bleeding, even from minor bumps or falls.
The same risk applies to other blood thinners: aspirin, heparin, enoxaparin, dabigatran, rivaroxaban. The combination doesn’t just increase bleeding risk-it makes it unpredictable. You can’t tell when it’s happening until you start bruising easily, notice blood in your stool, or develop a headache that won’t go away.
Black Pepper Makes It Worse-A Lot Worse
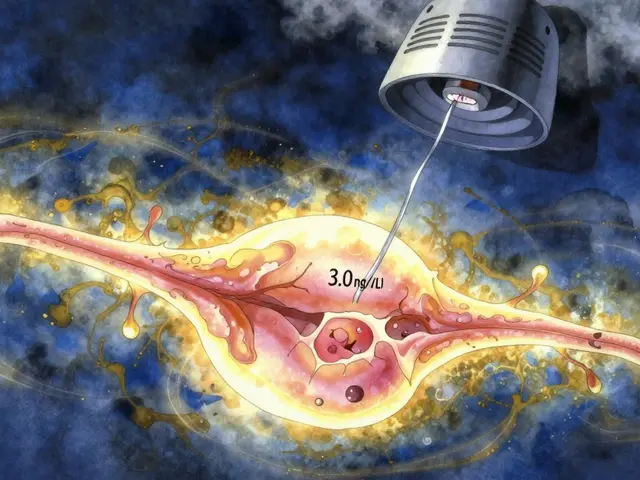
Here’s the twist: almost all turmeric supplements include black pepper extract. Why? Because piperine, the active compound in black pepper, boosts curcumin absorption by up to 2,000%. That sounds like a win-until you realize your body is suddenly flooded with curcumin levels it wasn’t designed to handle.Piperine doesn’t just help turmeric get absorbed. It also shuts down key liver enzymes (CYP3A4 and P-glycoprotein) that break down both curcumin and most blood thinners. That means your medication stays in your system longer than it should. Your warfarin dose, which was carefully calibrated, suddenly becomes too strong. Your apixaban doesn’t clear out as quickly. The result? A dangerous buildup of both substances in your bloodstream.
This isn’t theoretical. A 2023 study showed that high-dose curcumin increased clopidogrel blood levels in animals. Another small human trial found that curcumin made sulfasalazine (a drug for arthritis and colitis) reach 3.2 times higher concentrations in the blood. The same mechanism applies to blood thinners. And when you combine turmeric and black pepper? You’re not just doubling the risk-you’re multiplying it by ten or more.
Dietary Turmeric Is Fine. Supplements Are Not.
If you love turmeric in your curry, golden milk, or scrambled eggs, don’t panic. Eating turmeric as a spice is safe-even for people on blood thinners. Why? Because the amount you consume in food is tiny. A teaspoon of ground turmeric contains about 200 milligrams of curcumin. A typical supplement? 500 to 1,000 milligrams per capsule. And that’s before you add black pepper extract.Studies show that culinary use doesn’t affect INR levels or interfere with medication. But supplements? They’re concentrated, unregulated, and designed to flood your system. The difference isn’t just in quantity-it’s in intent. Food delivers nutrients slowly. Supplements deliver a drug-like punch.
One patient on Reddit reported no issues using turmeric in cooking while on apixaban. Another reported a hospital visit after taking one teaspoon of turmeric supplement daily for three weeks. The difference? One was in food. The other was in a pill.
What the Experts Say
Major medical groups are united on this:- The Cleveland Clinic says: "Avoid turmeric supplements if you’re on blood thinners. The risk of serious bleeding is real and well-documented."
- The Welsh Medicines Advice Service updated its guidance in October 2024, warning that turmeric can interfere with warfarin’s narrow therapeutic window-the small range between effective and toxic doses.
- The American College of Cardiology updated its 2024 guidelines to explicitly recommend complete avoidance of turmeric supplements in patients taking warfarin and cautious use with other anticoagulants.
- The British Heart Foundation advises: "Check with your GP before taking any herbal supplement, especially if you have heart disease or are on anticoagulants."
Even when turmeric is labeled as "natural" or "herbal," it’s still a powerful substance that interacts with your body’s chemistry. Natural doesn’t mean safe-especially when you’re already on medication.
Hidden Dangers Beyond Bleeding
The risks don’t stop at bleeding. Turmeric supplements, especially those with black pepper, have been linked to liver damage. Symptoms include:- Dark urine
- Yellowing of skin or eyes (jaundice)
- Nausea, vomiting, or loss of appetite
- Unusual fatigue or weakness
- Stomach or abdominal pain
These symptoms can appear within 2 to 12 weeks of starting the supplement. In one case, a patient developed acute liver injury after taking a turmeric-black pepper capsule daily for six weeks. Their liver enzymes spiked to three times the normal level. They required hospitalization.
And it’s not just about the ingredients. A 2022 ConsumerLab analysis found that 30% of turmeric supplements tested contained lead levels exceeding California’s safety limits. Heavy metal contamination is common in supplements sourced from countries with weak regulation. You’re not just risking drug interactions-you might be poisoning yourself.

What Should You Do?
If you’re on a blood thinner:- Stop taking turmeric supplements immediately. This includes capsules, powders, tinctures, and "enhanced" formulas with black pepper.
- Don’t assume "natural" is safe. Supplements aren’t tested like drugs. Labels can be misleading or incomplete.
- Check your bottle. If it says "with black pepper," "bioavailable," or "absorption boosted," it’s high-risk.
- Talk to your doctor or pharmacist. Even if you’ve been taking it for years, they need to know. A 2022 JAMA study found 42% of patients never tell their doctor about supplement use.
- Stick to food. A teaspoon of turmeric in your cooking is fine. Avoid concentrated doses.
If you’ve been taking turmeric supplements and notice any signs of bleeding-easy bruising, nosebleeds, blood in urine or stool, prolonged bleeding from cuts-seek medical help right away. Don’t wait.
What About Other Supplements?
Turmeric isn’t the only one. Other supplements that can interact with blood thinners include:- Ginger
- Ginkgo biloba
- Garlic supplements
- Green tea extract
- Fish oil (high doses)
- St. John’s Wort
Just because something is sold in a health food store doesn’t mean it’s safe with your meds. Always ask your pharmacist to review your full supplement list-every pill, powder, and tincture.
Looking Ahead: Is Anything Changing?
The market for turmeric supplements is huge-$1.14 billion in the U.S. in 2022. And 63% of those products include black pepper. But regulators are starting to take notice. The FDA’s 2022 database showed that only 41% of turmeric supplements carry warnings about blood thinner interactions, even though they’re legally required to.Research is underway to find safer forms of curcumin-like ones bound to lecithin-that deliver benefits without the dangerous absorption spike. But those aren’t on the market yet. Until then, the safest choice is simple: avoid the combo.
If you want the anti-inflammatory benefits of turmeric, get them from your kitchen-not your medicine cabinet. And if you’re on a blood thinner, treat supplements like you would a new prescription: ask first, never assume.
Can I take turmeric spice in food if I’m on blood thinners?
Yes, using turmeric as a spice in cooking is generally safe. The amount you consume in food-like a teaspoon in curry or soup-is too low to interfere with blood thinners. The risk comes from concentrated supplements, not culinary use.
Does black pepper alone affect blood thinners?
Black pepper by itself doesn’t thin the blood. But the piperine in it blocks liver enzymes that break down many medications-including blood thinners. This causes those drugs to build up in your system, raising the risk of bleeding. So while black pepper isn’t the problem alone, it makes turmeric supplements far more dangerous.
How long does it take for turmeric to affect blood thinners?
Effects can show up in as little as a few days, but most cases of dangerous INR spikes or liver issues appear within 2 to 6 weeks of daily supplement use. That’s why many people don’t realize the problem until it’s serious.
What should I do if I’ve been taking turmeric supplements with my blood thinner?
Stop taking the supplement immediately. Contact your doctor or pharmacist to discuss your medication and whether you need an INR test or other blood work. Don’t wait for symptoms. Even if you feel fine, the interaction may already be happening.
Are there any turmeric supplements that are safe with blood thinners?
No. All turmeric supplements contain concentrated curcumin, and most include black pepper to boost absorption. Even those labeled as "piperine-free" may still have enough curcumin to interfere with your medication. Until research confirms a truly safe formulation, avoid all supplements.
Why don’t supplement labels warn about blood thinner interactions?
By law, supplement labels should include warnings for known drug interactions. But enforcement is weak. A 2022 FDA review found only 41% of turmeric supplements carry the required warning. Many companies ignore the rule, and consumers often don’t read labels anyway. Don’t rely on the label-ask your doctor.



Lana Kabulova
January 21, 2026 AT 15:14I took turmeric supplements for my arthritis for 8 months-no issues, right? Then I started bruising like a cartoon character. One day I sneezed and had a nosebleed that wouldn’t stop. Turned out my INR was at 7.8. I had no idea black pepper was in it. The label just said ‘enhanced bioavailability.’ No warning. No red flags. Just a pretty bottle. I’m lucky I didn’t bleed out in my sleep.
Chiraghuddin Qureshi
January 23, 2026 AT 05:47Brooo in India we use turmeric in everything-curry, milk, even on our skin 😎 But we never take it in pills. That’s like drinking gasoline because you like the smell of petrol. Food = safe. Pills = danger zone. 🚨 Also, black pepper? We use it to make turmeric work better in food, not to turn your liver into a dumpster fire. 🤦♂️
Ryan Riesterer
January 24, 2026 AT 10:36Curcumin inhibits platelet aggregation via COX-1 and thromboxane suppression. Piperine downregulates CYP3A4 and P-gp, significantly increasing the AUC of anticoagulants. The pharmacokinetic interaction is well-documented in vitro and in vivo. The clinical significance is non-trivial-especially in patients with narrow therapeutic index drugs like warfarin. Supplement regulation is a regulatory failure. FDA 21 CFR Part 111 is insufficient for this class of compounds.
Margaret Khaemba
January 25, 2026 AT 01:34I’m on apixaban and I LOVE turmeric in my golden milk-like, daily. But I stopped buying those ‘super turmeric’ capsules after reading this. I didn’t realize how much worse the black pepper made it. My pharmacist actually gave me a handout on this last month. So many people think ‘natural’ = ‘no side effects.’ It’s wild how little people know about what’s actually in these supplements. Thanks for sharing this-it could save someone’s life.
Brenda King
January 25, 2026 AT 22:05I’ve been telling my mom for years not to take those turmeric pills. She’s 72, on warfarin, and swears they help her knees. I showed her this article. She said ‘but it’s just a spice!’ I had to explain that a pill is like drinking 20 cups of curry. She finally agreed to stop. I’m so glad this info is out there. Please, if you’re on blood thinners-don’t risk it. Your body isn’t a lab rat.
Keith Helm
January 27, 2026 AT 14:19Stop. Immediately. Consult your physician. Document your supplement use. Do not delay.
Alec Amiri
January 28, 2026 AT 07:10LMAO people still take turmeric pills? 😂 Bro, you’re literally paying $30 for a fancy spice and then wondering why you’re bleeding out. Black pepper? That’s just the cherry on top of your stupid decision. Your liver is screaming. Your blood is thinning. And you’re still scrolling through Instagram ads for ‘organic turmeric with quantum absorption.’ Wake up. You’re not a wellness influencer. You’re a walking drug interaction.
Lauren Wall
January 28, 2026 AT 21:24So let me get this straight-people pay for something that’s literally a poison when combined with their meds, and then act surprised when they end up in the ER? I’m not even mad. I’m just disappointed.
Kenji Gaerlan
January 30, 2026 AT 20:20wait so black pepper is bad? i thought it was just spicy? lol i took that turmeric thing for 2 months and i feel fine… maybe its just my body? 🤷♂️
Akriti Jain
January 31, 2026 AT 12:43Of course the FDA doesn’t warn you. 🤭 They’re in bed with Big Supplement. You think they want people knowing that 30% of turmeric pills have lead? That the ‘natural’ label is a scam? That your ‘wellness guru’ is selling you a time bomb? Wake up. This isn’t an accident. It’s a profit-driven massacre. And they’re counting on you to be too lazy to read the fine print. 💀