When you hear PSA test, you might think it’s a simple yes-or-no answer about prostate cancer. But the truth is messier. A high PSA number doesn’t mean you have cancer. A low one doesn’t guarantee you’re safe. And too many men end up with unnecessary biopsies, months of anxiety, and treatments they never needed-all because the test is misunderstood.
What PSA Testing Really Tells You (And What It Doesn’t)
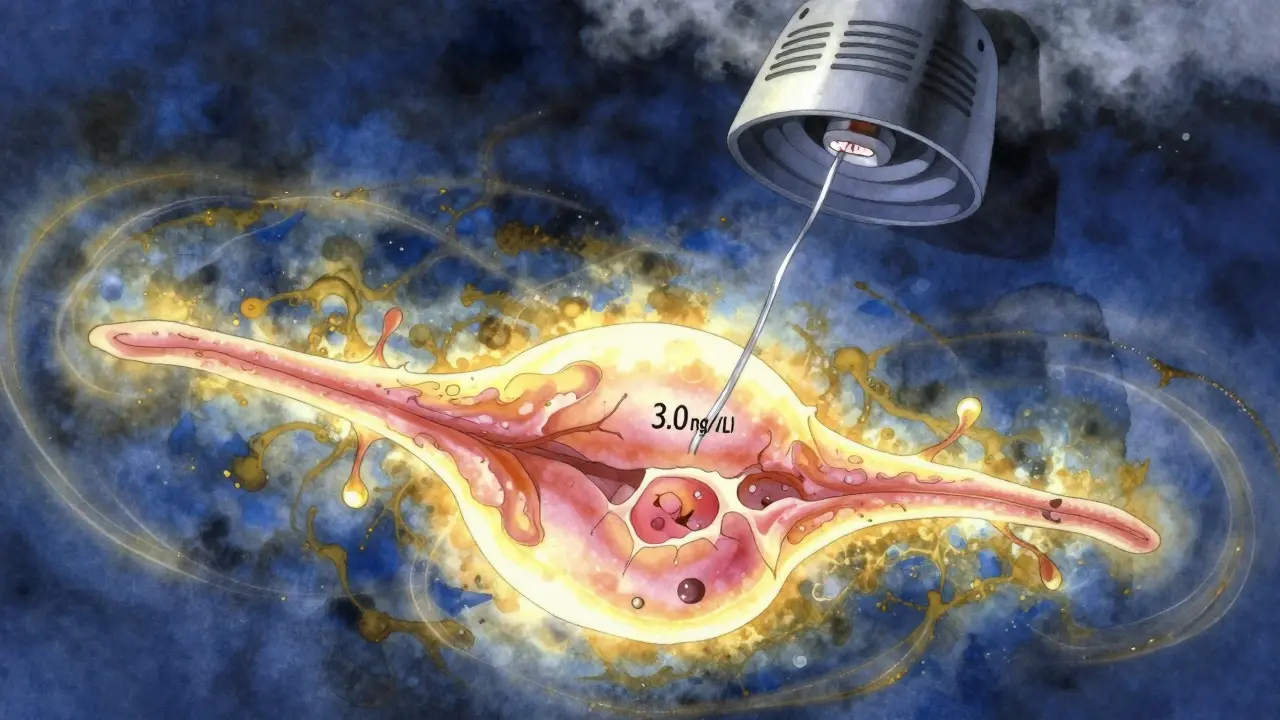
The PSA test measures prostate-specific antigen, a protein made by the prostate gland. It’s not a cancer test. It’s a signal. Think of it like a smoke alarm: it goes off when something’s wrong, but it doesn’t tell you if it’s toast burning or a house on fire.
For decades, doctors used 4.0 ng/mL as the cutoff. If your PSA was above that, you got referred for a biopsy. But research since 2020 has shown this threshold misses cancers in younger men and over-treats older men. Today, the National Comprehensive Cancer Network (NCCN) recommends acting when PSA hits 3.0 ng/mL. The European Association of Urology still leans on risk-based decisions, not fixed numbers.
Here’s the hard part: at a 4.0 ng/mL cutoff, only about 1 in 4 men with elevated PSA actually have prostate cancer. That means 75% of those biopsies are for nothing. And if you drop the threshold to 2.5 ng/mL to catch more cancers, you double the number of false alarms. The test is sensitive-it catches most cancers-but it’s terrible at telling which ones matter.
Age matters too. A PSA of 5.0 might be normal for a 70-year-old but raise red flags for a 50-year-old. Still, age-adjusted ranges aren’t perfect. A Duke University study found Black men with PSA between 3-4 ng/mL are over 2 times more likely to get a biopsy than White men with the same number-yet they’re 18% less likely to have cancer. This isn’t just a medical issue. It’s a racial equity issue.
The Biopsy Dilemma: When It’s Necessary and When It’s Not
A biopsy is the only way to confirm prostate cancer. But it’s invasive. You’ll have needles inserted through your rectum or perineum. There’s a 1 in 20 chance of infection. Bleeding. Discomfort that lasts days. And if your PSA was high for no good reason? You’ve gone through all that for nothing.
That’s why smart doctors don’t rush to biopsy anymore. They look at trends. Did your PSA jump from 2.1 to 3.8 in a year? That’s more worrying than a steady 3.5. They check for free PSA-how much of the total PSA is unbound. Lower free PSA means higher cancer risk. Some clinics now use advanced tests like the 4Kscore or Prostate Health Index (PHI). These combine PSA with other proteins and give a percentage risk of aggressive cancer. They’re more accurate than standard PSA alone, especially in the 2-10 ng/mL range where things get murky.
But here’s the catch: these tests cost $300-$450. Insurance often requires prior authorization. Medicare covers them, but not all private plans do. Many men never even hear about them because their doctor never mentioned alternatives.
And then there’s MRI. Multiparametric MRI (mpMRI) can show suspicious areas in the prostate without needles. If the MRI looks clean, you might avoid biopsy entirely. The PICTURE trial, with results expected in 2024, is testing whether starting with MRI instead of PSA could cut unnecessary biopsies by half. Early data shows an MRI-negative result has a 91% negative predictive value-meaning if your MRI is clear, you’re extremely unlikely to have dangerous cancer.
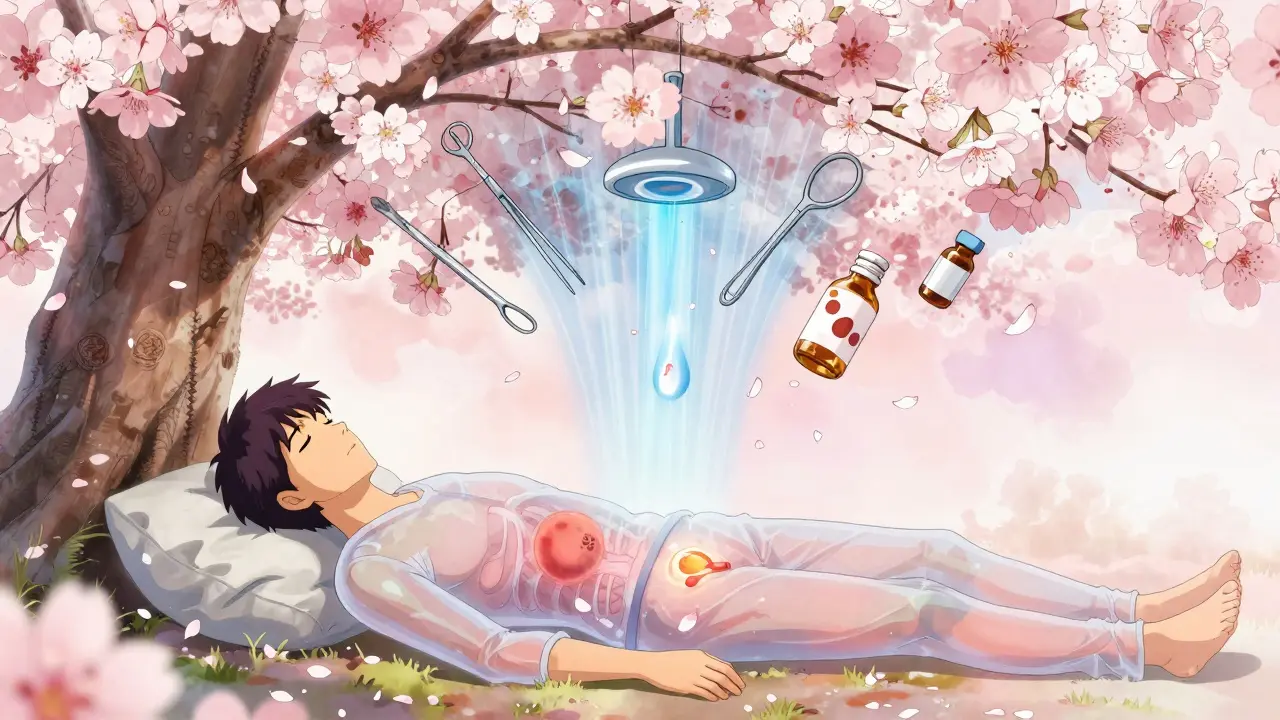
Treatment Options: Not Every Cancer Needs to Be Treated
Once cancer is confirmed, the next question isn’t always “What’s the best treatment?” It’s “Does this cancer even need treatment?”
Prostate cancer grows slowly. Many tumors are so low-risk they’ll never cause symptoms or shorten your life. But once you’re diagnosed, the pressure to act is real. That’s why active surveillance is now the standard for low-grade cancer (Gleason 6 or ISUP Grade Group 1). You get regular PSA tests, MRIs, and repeat biopsies-not to cure, but to watch. If the cancer stays quiet, you live normally. If it changes, you intervene.
For men who do need treatment, options include:
- Radical prostatectomy: Surgical removal of the prostate. Recovery takes weeks. Risk of incontinence (5-15%) and erectile dysfunction (30-60%) depends on age, nerve-sparing technique, and surgeon skill.
- External beam radiation: Daily treatments over 7-9 weeks. Less invasive than surgery, but side effects like bowel irritation and urinary problems can last months.
- Brachytherapy: Radioactive seeds implanted in the prostate. Shorter treatment time, but can cause urinary blockage.
- High-intensity focused ultrasound (HIFU) and cryotherapy: Less common, still being studied. Used mostly for men who can’t have surgery or radiation.
For advanced cancer, hormone therapy (androgen deprivation therapy) is often used to starve cancer cells of testosterone. It works-but side effects include hot flashes, weight gain, bone thinning, and loss of libido. Newer drugs like enzalutamide and apalutamide extend survival but come with higher costs and risks.
The biggest mistake? Treating low-risk cancer like it’s life-threatening. A 2022 study in Urology Practice found 62% of men felt misled by their initial PSA results. Many thought a diagnosis meant they had to rush into surgery or radiation. But for low-grade tumors, waiting is often the safest choice.
Who Should Be Screened-and When
The U.S. Preventive Services Task Force says men aged 55 to 69 should make an individual decision about PSA screening after talking with their doctor. That’s not a recommendation to screen. It’s a recommendation to decide.
Men at higher risk-Black men, those with a father or brother diagnosed before 65, or those with BRCA gene mutations-should start earlier. The American Urological Association suggests a baseline PSA at age 40-45. That first number becomes your personal benchmark. A 4.0 at 45 is very different from a 4.0 at 65.
Screening every year isn’t necessary for everyone. If your PSA is under 2.5 and you’re healthy, testing every 2-4 years is often enough. If it’s rising, you might need annual checks. The goal isn’t to catch every tiny cancer. It’s to catch the ones that could kill you.
What You Can Do Right Now
If you’re considering PSA testing:
- Ask your doctor: “What’s my risk based on my age, race, and family history?”
- Request a discussion about benefits and harms. It should take at least 15 minutes. If your doctor rushes you, find someone who won’t.
- If your PSA is above 3.0, ask: “Can I get a free PSA test or 4Kscore before a biopsy?”
- If you’re told you have low-grade cancer, ask: “Is active surveillance an option?” Don’t assume surgery is the only path.
- Ask about MRI. Many hospitals now offer it as part of the diagnostic process.
Don’t let fear drive your choices. Prostate cancer screening isn’t about eliminating risk. It’s about managing it. The goal isn’t to live longer-it’s to live well. And that means avoiding unnecessary procedures as much as catching the real threats.
What’s Changing in 2026
The field is shifting fast. The IsoPSA test, which looks at PSA shape instead of just quantity, showed 95% specificity in 2022 trials. AI tools are being trained to predict cancer risk from PSA trends over time, replacing fixed thresholds. PSMA-PET/CT scans are becoming more common for staging advanced disease, though they’re still expensive and not widely available.
By 2028, experts predict a 30% drop in unnecessary biopsies thanks to better risk tools. The future isn’t more testing. It’s smarter testing.
What matters isn’t the number on the lab slip. It’s the conversation you have after it.
Is a high PSA level always a sign of prostate cancer?
No. A high PSA can be caused by many things: an enlarged prostate (BPH), infection, recent ejaculation, cycling, or even a digital rectal exam. PSA levels naturally rise with age. Only about 25% of men with elevated PSA end up being diagnosed with prostate cancer after biopsy. That’s why follow-up tests and risk assessments are crucial before jumping to conclusions.
Should I get a PSA test if I’m over 70?
For most men over 70, routine PSA screening isn’t recommended unless they’re in excellent health and have a life expectancy of more than 10-15 years. Prostate cancer often grows so slowly that it won’t affect men in their 70s or 80s. The risks of overdiagnosis and treatment side effects usually outweigh the benefits at this age. Talk to your doctor about your personal situation.
What are the side effects of prostate cancer treatment?
Treatment side effects vary. Surgery and radiation can cause urinary incontinence (up to 15%), erectile dysfunction (30-60%), and bowel issues. Hormone therapy leads to hot flashes, fatigue, weight gain, and bone loss. Even active surveillance carries psychological stress. The key is matching treatment to cancer risk-low-grade tumors rarely need aggressive treatment, which reduces the chance of unnecessary side effects.
Why do Black men have higher biopsy rates but lower cancer detection?
Black men tend to have higher PSA levels naturally, even without cancer. When doctors use the same cutoffs for all men, Black men are more likely to be flagged for biopsy. Studies show they’re 2.3 times more likely to get a biopsy with PSA between 3-4 ng/mL, but 18% less likely to have cancer confirmed. This points to a need for race-specific risk models and better biomarkers to reduce disparities in care.
Can I avoid a biopsy if my PSA is elevated?
Yes, in many cases. Advanced tests like the 4Kscore or PHI can give a clearer picture of cancer risk without a biopsy. If your MRI scan shows no suspicious areas, you may be able to delay or avoid biopsy entirely. Active surveillance is also an option for low-risk cases. Ask your doctor if these alternatives are available and covered by your insurance.
What’s the difference between active surveillance and watchful waiting?
Active surveillance is for men with low-risk cancer who are monitored closely with regular PSA tests, MRIs, and repeat biopsies. The goal is to catch any progression early and treat it before it spreads. Watchful waiting is less intensive and typically for older men or those with other health issues. It focuses on managing symptoms rather than curing cancer. Active surveillance is more common today for healthy men with low-grade tumors.



Katherine Carlock
January 13, 2026 AT 05:36PSA is such a flawed tool but we keep treating it like gospel. I had a 4.8 last year and spent three months terrified until my urologist ordered a 4Kscore-it came back at 7% risk. No biopsy. Just monitoring. Why isn’t this standard everywhere?
Sonal Guha
January 15, 2026 AT 01:37Black men get biopsied more but have less cancer what a joke the system is rigged the doctors dont care about data they care about billing
Prachi Chauhan
January 16, 2026 AT 05:57It’s funny how we treat a protein level like a moral verdict. PSA isn’t truth-it’s noise. We’ve turned medicine into a numbers game instead of a human conversation. What if we stopped chasing numbers and started listening to bodies? Not every alarm needs a firetruck.
Jennifer Phelps
January 17, 2026 AT 08:52I read that Duke study about Black men and PSA and I just sat there I mean how many people are getting biopsies for nothing because we use the same cutoff for everyone
Alice Elanora Shepherd
January 17, 2026 AT 22:01Active surveillance is so underutilized. I’ve seen patients panic after a Gleason 6 diagnosis-yet their cancer is statistically harmless. The real tragedy isn’t the cancer-it’s the fear we don’t properly manage. Doctors need to spend more time explaining risk, not just handing out referrals.
Jessica Bnouzalim
January 19, 2026 AT 07:50My dad had a PSA of 6.2 at 72 and they wanted to do a biopsy right away… I made them wait. Got an MRI first-clean as a whistle. He’s 75 now and fine. Why do we still treat every number like a death sentence??
TiM Vince
January 20, 2026 AT 17:09In India, most men don’t even know what PSA stands for. I showed my uncle the article-he’s 62, never seen a urologist. We need to make this info accessible, not just for people who Google it. Education is the real screening tool.
gary ysturiz
January 20, 2026 AT 20:41Thank you for writing this. I was one of those guys who thought a high PSA meant I had cancer and rushed into surgery. Turns out I had BPH. I lost six months of my life to fear. Please, if you’re reading this-ask for the 4Kscore. Ask for the MRI. Don’t let anyone rush you. You have time. Your life matters more than a number.
laura manning
January 22, 2026 AT 10:07While the article presents a compelling argument against overtesting, it lacks sufficient citation of longitudinal outcome data regarding active surveillance cohorts. The 2022 Urology Practice study referenced, while informative, does not account for selection bias in patient cohorts. Furthermore, the economic implications of widespread MRI adoption remain underexplored, particularly in fee-for-service healthcare models.
Sona Chandra
January 23, 2026 AT 19:02THIS IS WHY MEN DIE. YOU LET A NUMBER DECIDE YOUR LIFE?? YOU’RE NOT A STATISTIC. YOU’RE A MAN. IF YOUR PSA IS UP-GO GET THE BIOPSY. DON’T WAIT. DON’T ASK FOR MRIs. DON’T PLAY GAMES. IF YOU’RE AFRAID, YOU’RE ALREADY LOSING.
Lawrence Jung
January 24, 2026 AT 11:43People think medicine is about facts but it’s about power. Who controls the test controls the fear. PSA was never about health. It’s about keeping the machine running. Biopsies. Treatments. Drugs. All profitable. The truth? Most prostate cancers die with you. Not because you treated them. Because they were never the enemy.